AUCTORES
Globalize your Research
case report | DOI: https://doi.org/10.31579/2690-4861/462
1Department of Plastic and Reconstructive Surgery, MedStar Georgetown University Hospital; Washington, District of Columbia.
2Department of Plastic and Reconstructive Surgery, Georgetown University School of Medicine; Washington, District of Columbia.
3Plastic and Reconstructive Surgery Division, Rutgers Robert Wood Johnson Medical School, New Brunswick, New Jersey.
4Department of Surgery, University of Pittsburgh Medical Center (UPMC) Mercy Hospital, Pittsburgh, Pennsylvania.
5Division of Plastic and Reconstructive Surgery, Department of Surgery, Keck School of Medicine, University of Southern California, Los Angeles, California.
6Department of Plastic and Reconstructive Surgery, MedStar Washington Hospital Center; Washington, District of Columbia.
*Corresponding Author: Laura K. Tom, MD, Department of Plastic and Reconstructive Surgery MedStar Washington Hospital Center 106 Irving Street NW Washington DC, 20010.
Citation: Daisy L. Spoer, Lauren E. Berger, Parhom N. Towfighi, Karen R. Li, Laura K. Tom, (2024), Surgical Techniques for Lymphovenous Bypass: A Review, International Journal of Clinical Case Reports and Reviews, 17(5); DOI:10.31579/2690-4861/462
Copyright: © 2024, Laura K. Tom. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 26 April 2024 | Accepted: 16 May 2024 | Published: 13 June 2024
Keywords: lymphatic vessels; microsurgery; lymphedema; lymphovenous bypass; lymphovenous anastomosis
Background: Lymphedema is a progressive, debilitating disease that may affect up to 250 million individuals worldwide. Complex decongestive therapy (CDT) remains the first line of treatment for lymphedema, and surgical treatment currently has no formally established role. In recent years, lymphovenous bypass (LVB) has emerged as a potentially efficacious intervention to improve patients' objective and subjective measures of lymphedema. Despite this promise, there are few evidence-based recommendations to inform the adoption of the practice.
Methods: A narrative review of the present literature on LVB was performed through a query of records using various combinations of Medical Subject Heading (MeSH) terms and keywords such as “lymphatic vessels,” “lymphedema,” “breast cancer lymphedema,” “surgical anastomosis,” “lymphovenous bypass,” “lymphovenous anastomosis.” The articles were assessed for 1) bibliometric characteristics, 2) preoperative evaluation, 2) operative techniques, 3) postoperative regimens, and 4) outcome measures.
Results: The sixty-year evolution of LVB has transformed rapidly in response to technological advances in the last two decades. The geographically distributed investigation of these surgical innovations has prompted a fragmentation of LVB practice. As original research outpaces literature review, there needs to be more consistency in terminology, perioperative practices, and evaluation of outcomes of LVB, which challenge systematic analysis. The systematic reviews to date emphasize the ability of LVB to improve objective measures such as limb circumference. Still, the inconsistent use of subjective measures limits our appreciation of the collective improvement in patient-reported outcomes. Moreover, there are a limited number of accepted methods for patient selection, preoperative evaluation, and surgical planning, with many surgical techniques employed.
Conclusion: The unifying principles and scientific evidence must be clarified to guide an overarching consensus before the widespread adoption of LVB. This article aims to synthesize recommendations and current institutional preferences concerning the research and clinical applications of LVB. The collaboration and continued refining of these practices will be necessary to establish the role of LVB in the treatment and prevention of lymphedema.
Lymphedema is a progressive, debilitating disease that may affect up to 250 million individuals worldwide. [1] In the industrialized world, secondary lymphedema often develops as a sequela of surgery, radiation, and chemotherapy in cancer treatment.[2-6] Inflammation due to surgery or chemotherapy can induce exudation of lymphatic free fatty acids and promote adipogenesis.[4,7-9] Synergistically, radiotherapy causes direct DNA damage and the release of reactive oxygen species that promote time-dependent degeneration.[10-12] The associated fibrosis and adipogenesis contribute to afterload-mediated lymphatic remodeling and dysfunction like hypertensive cardiomyopathy. [4,13-17] The disease is generally progressive, hastened by obesity, and results in reduced quality of life for up to 10 years.[18]
Complex decongestive therapy (CDT) is the standard approach to lymphedema management, but routine manual drainage and compression offer limited efficacy while carrying an immense treatment burden with inconsistent insurance coverage.[19-24]
The rising survivorship may predict increases in breast cancer-related lymphedema, and surgical innovations may offer solutions for preventing or mitigating the morbidity of this condition. Lymphovenous bypass is a physiological intervention that ideally prevents lymphedema progression by increasing collateral lymphatic outflow. Today, the advances in imaging and supermicrosurgical LVB confer an average decrease of 4.1 cm in limb volume and improve the quality-of-life measures in 57-100% of patients.[25-30]
Despite scientific evidence that LVB can improve subjective and objective outcomes of lymphedema beyond CDT, the marked heterogeneity of practice limits the widespread adoption.6,19,20,27-42 This narrative review aims to provide an overview of current LVB research, perioperative practices, and outcome measures to highlight essential gaps in the distributed investigation of LVB, which warrant further study and consensus.
Study Design
A literature search through December 2022 was performed across PubMed, the Web of Science, and Grey literature. A list of predetermined Medical Subject Heading (MeSH) search terms and keywords were employed, including but not limited to various combinations of the following: “lymphatic vessels,” “lymphedema,” “breast cancer lymphedema,” “surgical anastomosis,” “lymphovenous bypass,” “lymphovenous anastomosis” and the Boolean operators “AND” and “OR,” disregarding results for non-English language. Following record screening, the remaining studies then underwent full-text review. No restrictions were set on the year of publication, country of origin, or study size. This review's inclusion depended on predefined inclusion and exclusion criteria to select original and review articles on lymphovenous bypass. Studies assessing all physiologic lymphedema surgery were included only if outcomes of interest were stratified by procedure to understand the specific role of LVB better. Articles describing other surgical interventions, such as vascularized lymph node transfer or non-physiologic lymphatic surgery without cases of LVB, were also excluded. Full-text studies were included in this narrative review if they reported on the outcomes of interest. The articles were assessed for 1) bibliometric characteristics, 2) preoperative evaluation, 2) operative techniques, 3) postoperative regimens, and 4) outcome measures. Bibliometric data included information related to the terminology used, research era, and study location. Preoperative evaluation included data related to diagnosis and imaging. Operative techniques included data about instruments, vessel selection, bypass methods, and surgical training. The primary outcomes included clinical and patient-reported outcomes.
LVB Research and Nomenclature
The composite field of lymphedema research expanded within the last two decades (87.7%), of which surgery was the second most researched topic.6 Today, the leaders of lymphedema research span Australia, Belgium, China, Germany, Italy, Japan, the United Kingdom, the United States, and Taiwan.6 A recent bibliometric analysis of lymphedema research between 1900-2023 revealed that Japan had contributed the largest quantity of papers related to “lymphovenous anastomosis” and “microsurgery” (n=73 and 41 publications/year). The second most productive country for “lymphovenous anastomosis” was the United States (n=46 publications/year), which was tied with Italy as the second most productive in “microsurgery” (n=21 publications/year).6
A search of terms related to lymphatic surgical “bypass” (n=1093 PubMed results) and “anastomosis” (n=1,614 PubMed results) reveal trending parallel investigations on this surgical concept between 1964 and 2023 (n=2862 total PubMed results). The two fields of work may reflect distinct clusters of surgical study (i.e., microsurgical bypass and supermicrosurgical anastomosis) or inconsistent terminology.25,26,43-46 Coriddi et al. suggest using the term “lymphovenous bypass,” as it more accurately describes the “establishment of a shunt” than does the word “anastomosis,” which refers to a “communication between or coalescence of blood vessels.”47 This paper will discuss LVB as a unified topic.
Microsurgical Era (1960-1996)
The initial experimentation with LVB was facilitated by the advent of microsurgery in the 1960s, which permitted the surgical union of lymphatics to veins greater than 1 mm in diameter.48-52 These early models relied on dilated lymphatics and size-matched cutaneous veins for LVB, often impeded by 21 days postoperatively.50-55 In this era, lymphoscintigraphy was the gold-standard imaging modality for lymphedema, which necessitated ionizing radiation while offering low spatial and temporal resolution.
Supermicrosurgical Era (1997-Current)
In 1997, Koshima et al. demonstrated that surgical union of vessels < 0>1mm).57 These efforts have coincided with reports of improved patency at one week (70%), one month (65%), and one year (56.5%) post-procedure.58-60 The advances in imaging came shortly after that in 2001 with magnetic resonance lymphangiography (MRL) with gadolinium-based contrast, which increased the precision of anatomical staging and treatment planning but was expensive, resource-intensive, and potentially impractical for perioperative use.61 Finally, in 2007, indocyanine green (ICG) lymphography combined with near-infrared imaging (near-infrared fluorescence lymphangiography, [NIRF-L]) surfaced as a practical and more affordable functional imaging modality capable of real-time lymphatic mapping to highlight location, drainage directionality, and collateral circulation.62 The lymphatic uptake of ICG in NIRF-L allowed for visualization that ultimately informed the concept of lymphatic territories (“lymphosomes”).63
Patient Selection
A lymphedema diagnosis can be determined by a change in volume measures, bioimpedance spectroscopy, a physical exam, and clinical history. Still, it may be enhanced by additional measures of lymphoscintigraphy, ultrasound, ICG fluoroscopy, or lymphography and classification systems (e.g., International Society of Lymphology staging criteria (ISL).20,64-73
The management of lymphedema differs by lymphedema stage and, in the surgical literature, often follows a stepwise application of CDT, LVB, and vascularized lymph node transfer (VLNT) with and without debulking surgery for less severe, partially obstructed, and severely obstructed lymphatics, respectively.27 There is a rationale to recommend LVB before VLNT as LVB is a less invasive procedure and more effective in early-stage disease.27,36,39,74-76 A failure of conservative management is not an absolute prerequisite for physiologic surgery, and in patients with breast cancer, those with ≥ 10% volume change should be referred to specialist care.77
Surgical Planning
Objective parameters of the abnormal lymphatic form (i.e., normal, dilated, or collaterals) or function (i.e., dermal backflow [DBF] or increased lymphatic transit time [TT]) are frequently integrated into the staging of lymphedema and are predictive of LVB outcomes. The current recommendation is to incorporate imaging-based modalities with a clinical assessment to characterize the severity of lymphedema and target surgical intervention more effectively. In cases of a nonfunctioning lymphatic system (NIRF-L +/- MRL) and pitting lymphedema, some recommend 1) intensive rehabilitation therapy followed by 2) reassessing the possibility of a reductive surgical technique.78,79 A functioning lymphatic system (NIRF-L +/- MRL) with a good axillary status may indicate LVB. In contrast, an axilla with fibrotic tissue or signs of radiodermatitis may indicate VLNT with fibrotic release combined with distal LVB. 79 A VLNT can be combined with free tissue transfer and LVB for individuals pursuing simultaneous breast reconstruction.79,80
NIRF-L, when combined with staging scales (e.g., the Koshima ICG Classification System, MD Anderson Cancer Center (MDACC) scale, and the Dermal Backflow Scale (DBS)), is considered the “gold standard” imaging modality for the diagnosis, severity staging, and surgical planning of LVB (Figure 2).31,46,81-86 The perioperative use of NIRF-L permits precise lymphatic mapping and is more predictive of outcomes than ISL.87,88 Adjunctive ultra-high-frequency ultrasound or “rest/stress intradermal lymphoscintigraphy” may enhance NIRF-L sensitivity.44,89-91
MRL is more sensitive than NIRF-L and may be suitable for cases warranting a more detailed visualization of the deep lymphatic system (>2 cm deep to the skin surface) and surrounding tissue characteristics.31 The increased sensitivity can paradoxically influence inaccurate surgical planning and is often considered impractical due to the financial costs. New frontiers include high-frequency ultrasound imaging and photoacoustic imaging (PAI), both of which are praised for their sensitivity and, in combination with clinical presentation, have the potential to aid in the expansion of LVB indications.31,92,93

Figure 1. Overview of lymphatic and venous vasculature frequently used in LVB. The caliber of lymphatics varies in the published literature, although they have been categorized into initial lymphatics (0.01-0.06 mm), pre-collector (0.035–0.150 mm), and collector lymphatics (0.200 mm).182,183 Thus, we illustrated a collector lymphatic as the relevant structure for LVB. (A) Collector lymphatics have tight “zipper-like” junctions, specialized muscle cells, and valves that coordinate directional lymph flow via suction-derived diastolic filling.3,15,172 (B) The cutaneous vessels used in LVB generally include valved subdermal venules (0.3-0.6mm) or large cutaneous veins (>1mm).57 The microcirculatory venules and veins vary according to their ultrastructure and anatomical location, and a venule with sparse smooth muscle cells is illustrated for generalizability.101,184,185
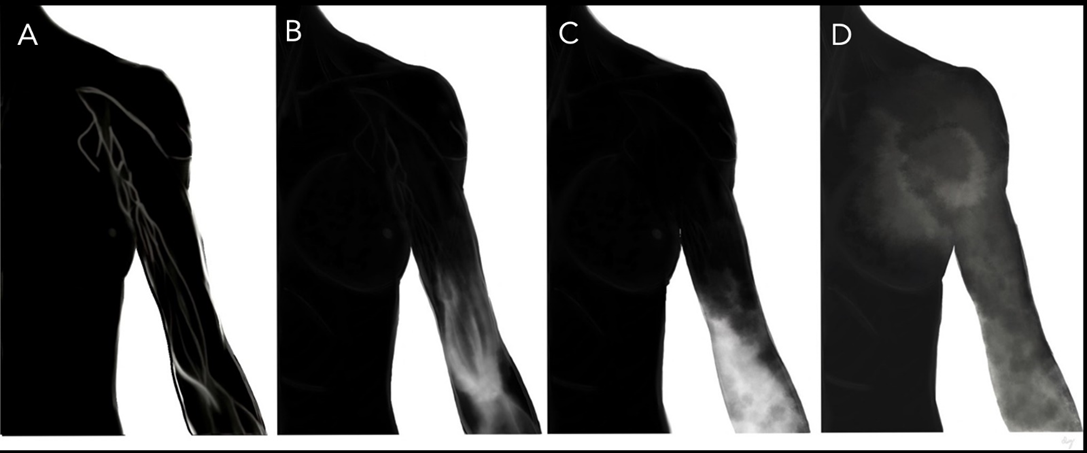
Figure 2. Patient selection and preoperative evaluation. Illustration of Koshima ICG lymphedema classification system.98 (A) Stage 0: “Normal superficial lymphatic vessels appear as a “linear” pattern with no dermal backflow” (B) Stage 1: “Lymphatic vessels appear dilated and torturous with areas of ICG accumulation as a “splash” pattern” (C) Stage 2: “Contracted lymphatic vessels with loss of intraluminal diameter and thickening of the smooth muscle cell coverage. Lymphatic vessels are disrupted, causing increased areas of ICG accumulation as a “stardust” pattern” (D) Stage 3: “No lymphatic vessels can be seen and there is ICG accumulation as a “diffuse” pattern.”98
Instruments
The preferred instruments for LVB vary and include either supermicrosurgical forceps (0.05 mm tips) or standard microsurgical forceps (0.3 mm). Some consider supermicrosurgical forceps too malleable to avoid damaging the lumen of the lymphatics. Titanium supermicrosurgical instruments and surgical scissors are generally employed.94
Selection of Target Lymphatics
Figure 3 illustrates the step-wise process for selecting target vessels. The lymphatic targets appropriate for bypass must be functional as there is evidence of little to no therapeutic benefit of performing LVB with sclerotic lymphatic vessels. The use of LVB has demonstrated objective and subjective improvement in the lower extremity (objective 46.7-100%, subjective 84-100%) and upper extremity (objective 0-100%, subjective 50-100%) lymphedema.28,29 Functional imaging (i.e., NIRF-L) is recommended for reverse lymphatic mapping. The functional vessels draining the affected distal extremity will appear bright under NIRF-L due to their uptake of ICG (1-2 mg) injected intradermally into the alternating web spaces of the impacted hand or foot.95,96 The fluorescence pattern will demonstrate the disease severity. Incisions are generally guided by dermal backflow (NIRF-L findings) and placed according to the mapped functional lymphatics.36,84,97,98 There is no consensus on the preferred incision length. Still, using the AccuVein system (AccuVein Inc.) in conjunction with NIRF-L, Mihara et al. performed the procedure through a 2-mm incision.45 Isosulfan blue (Lymphazurin; United States Surgical Corp., Norwalk, CT) or methylene blue (American Reagent, Shirley, NY) is helpful intraoperatively, as it allows for gross visualization of lymphatic patency and function (Figure 3). A functional lymphatic is thus frequently defined as both ICG-positive and flow-positive.

Figure A
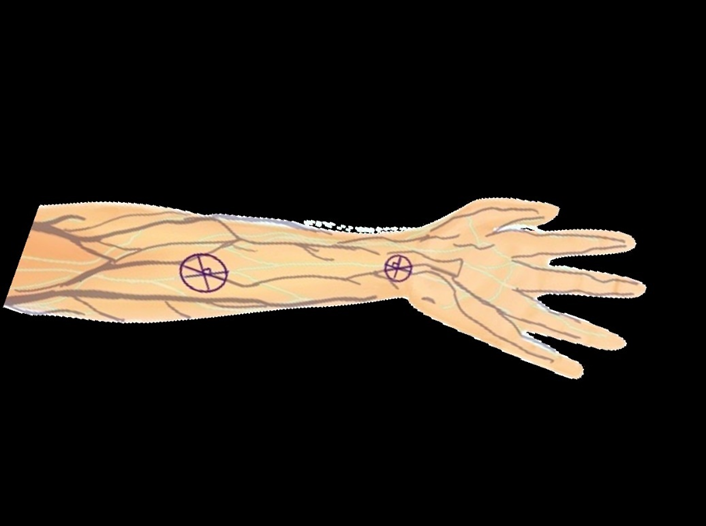
Figure B

Figure 3: Selection of lymphatic and venous targets. (A) The lymphatic territories (lymphosomes) can be visualized with ICG. Lymphosomes superior to inferior 1) temporal, purple; 2) occipital, blue; 3) mental, tan; 4) supraclavicular, pink; 5) subscapular, not pictured; 6) axillary, dark teal; 7) pectoral, orange; 8) superior inguinal, red; 9) lateral inguinal, salmon; 10) inferior inguinal, magenta; 11) popliteal, not pictured. [illustration of lymphosomes adapted from Suami et al.]186 (B) Pre-incision selection of target vessels will depend on the location of the obstruction and the presence of fluorescent lymphatics and neighboring veins. The incision should be placed over a junction between a lymphatic and vein (X and overlying circle). The incision can be made perpendicular to the lymphatic. Selecting several possible sites for incision is ideal (C) lymphatic and vein in preparation for LVB.
The fibrotic and pressure-overloaded lymphatic in the diseased state will dilate and exhibit ineffective lymphatic pumping.4,7,15 In a recent analysis of 1048 lymphatic vessels, Yang et al. extrapolated that 0.5 mm (lymphatic vessel0.5) represented the threshold for lymphatic function, with calibers ≤ 0.5 mm associated with an adequate function (defined as ICG and flow positive) and postoperative volume reductions.99
Selection of Recipient Veins/Venules
The pressure gradient, tension, and flow dynamics of the recipient vein (RV) are paramount for a successful bypass.100 An algorithmic approach to venule or venous selection can be based on (1) caliber match, (2) location, and (3) the presence of backflow.100,101 The original framework considered small RV (≤ 0.4-0.5mm) superior to larger RV in minimizing backflow. This theory potentially contradicts the traditional teaching that, in the supine position, the superior vena cava exhibits the lowest venous pressure as it drains into the right atrium (0-3mmHg) and is precipitously lowered by negative thoracic pressure during inspiration and by gravitational pull when standing.101,102 Conversely, peripheral venules have higher intraluminal pressures due to an increased net cross-sectional area and relative gravitational influences (hand: +35 mm Hg, foot: +90 mm Hg).103
One study evaluating RV of 1,000 LVBs of similar lymphatic characteristics classified RV according to Visconti flow dynamic classifications, which demonstrated that the smallest RV (≤ 0.4mm) were significantly associated with the least favorable outcomes of backflow and slack compared with medium (0.5-0.9mm) and large (≥ 1mm) RV.100 Matching the caliber of RV and lymphatics while minimizing LVB tension was informative on the final LVB configuration's influence on the outcomes. A physiologic evidence-based algorithm for venous choice is provided in the referenced work.101
LVB Technique: Configuration
Table 1 depicts the variety of available techniques for LVB from the published literature.43,104-106 The photographs in Figure 4 demonstrate the practical application of a sequence of methods. The relevance of alternative strategies is primarily addressed in the original papers and institutional care algorithms.94,107-109 The first described approaches to LVB drew inspiration from microsurgical anastomosis of blood vessels and included end-to-end (E-E) and end-to-side (E-S) configurations.94,110 However, the postoperative histological evaluation in that era demonstrated that E-E was associated with slight narrowing at the LVB site and that E-S LVB was more often disrupted due to inflammatory changes.51,101 E-E has remained the most prominent technique across institutions, with authors citing the relative ease of use in caliber matching and improved resistance to venous backflow compared to E-S.
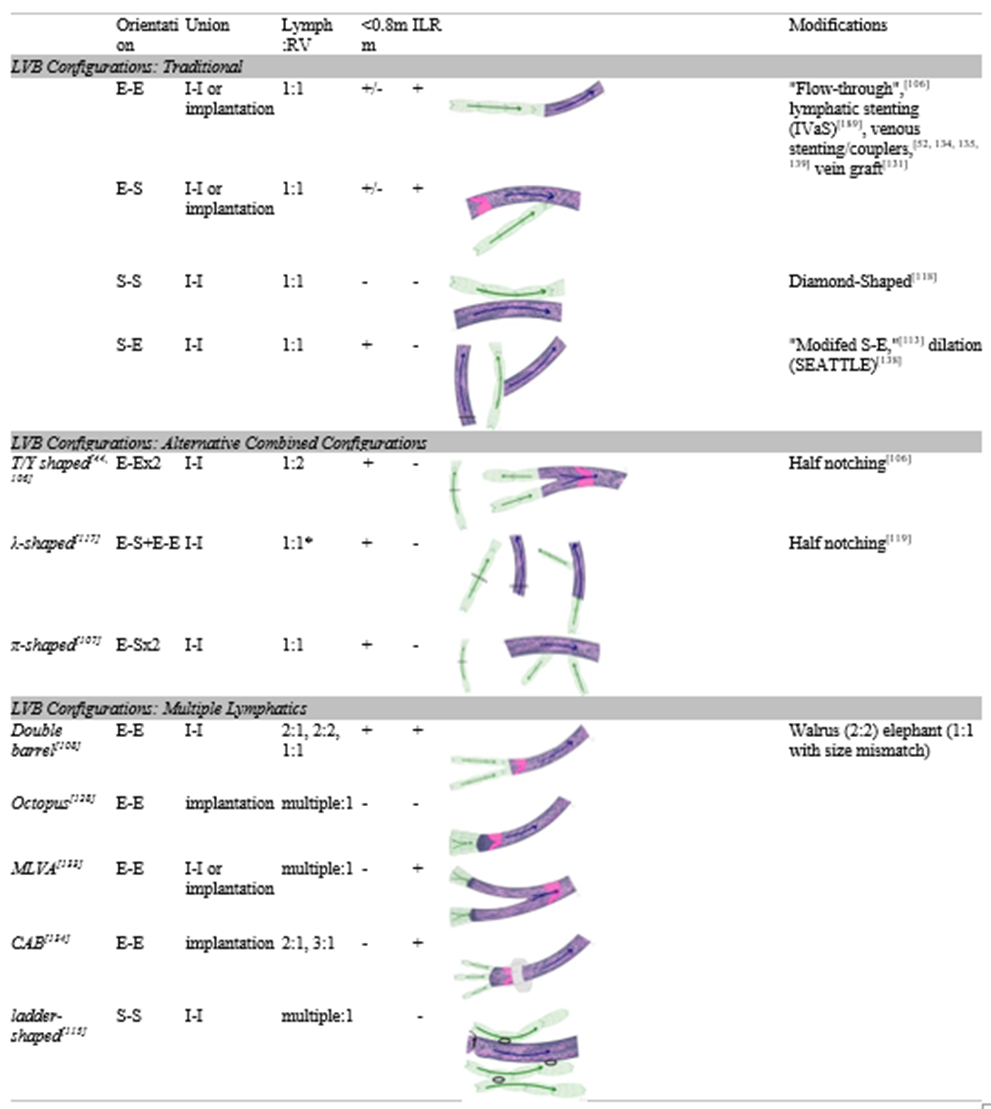
Table 1. Surgical Techniques for Lymphovenous Bypass. Depicts information and illustrations of LVB techniques as described in the published literature. The list is not comprehensive, and more options for LVB exist. Configurations are described by the direction of the union and include end-to-end (E-E), end-to-side (E-S), side-to-end (S-E), and side-to-side (S-S). Ratios of lymphatics: recipient veins (RV) comprise the number of individual, native lymphatics included in the LVB; lymphatics transected and employed using the proximal and distal ends were counted as one lymphatic. Ratios of 2:1 are described as λ-shaped, but the technique is described in the published literature as involving two ends of a transected lymphatic rather than a method of 2:1 LVB. Because procedures involving RV outlets <0>0.8, the procedure was marked with a “+/-.” Procedures that have been applied in the setting of immediate lymphatic reconstruction (ILR) were marked with a “+.” Illustrations are basic representations of the configurations drawn according to the procedural descriptions or images in the referenced articles. Lymphatics, valves, and direction of lymphatic flow (arrows) are depicted in green. RV and direction of flow (arrows) are displayed in dark blue; venous valves are in pink. The directionality of lymphatic flow was based on the orientation described in the technical articles, as lymphatics and RV have directional valves supporting flow in a distal to proximal manner. If the proximal or distal end of the lymphatic or vein was not specified, the directionality was depicted in the anatomical fashion, which would theoretically optimize flow. Modifications to the described approaches are listed with the procedures they are reportedly applied to.
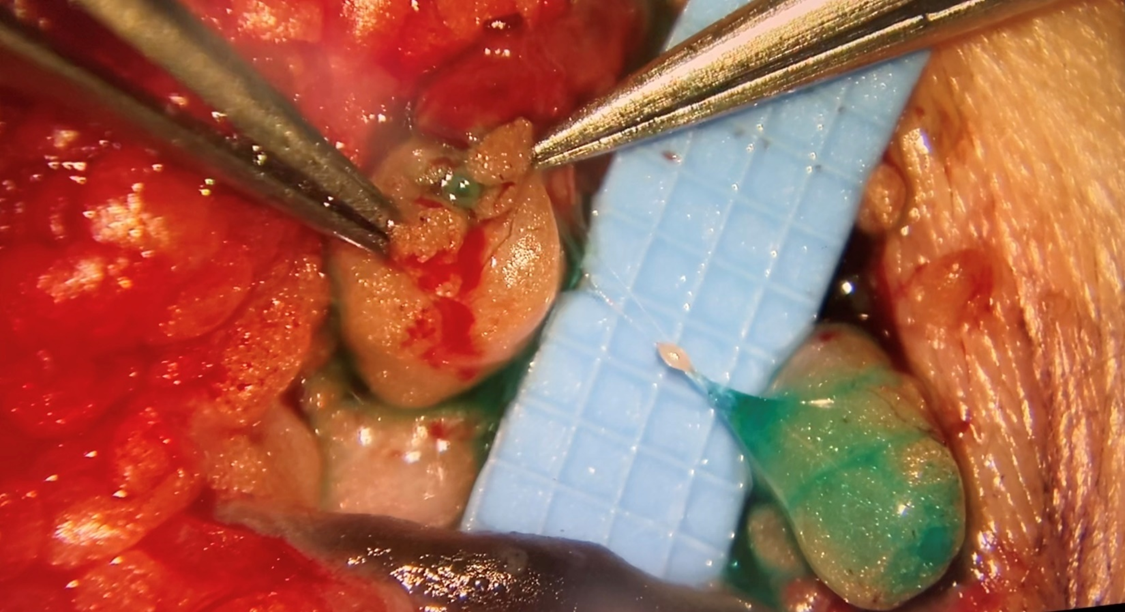
Figure 4A

Figure 4B
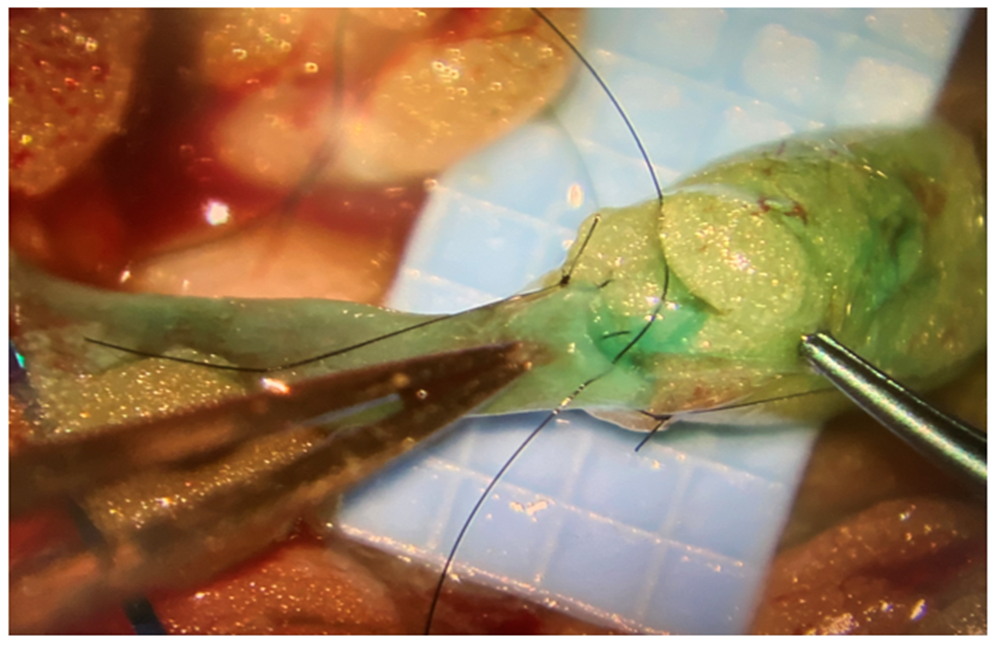
Figure 4C
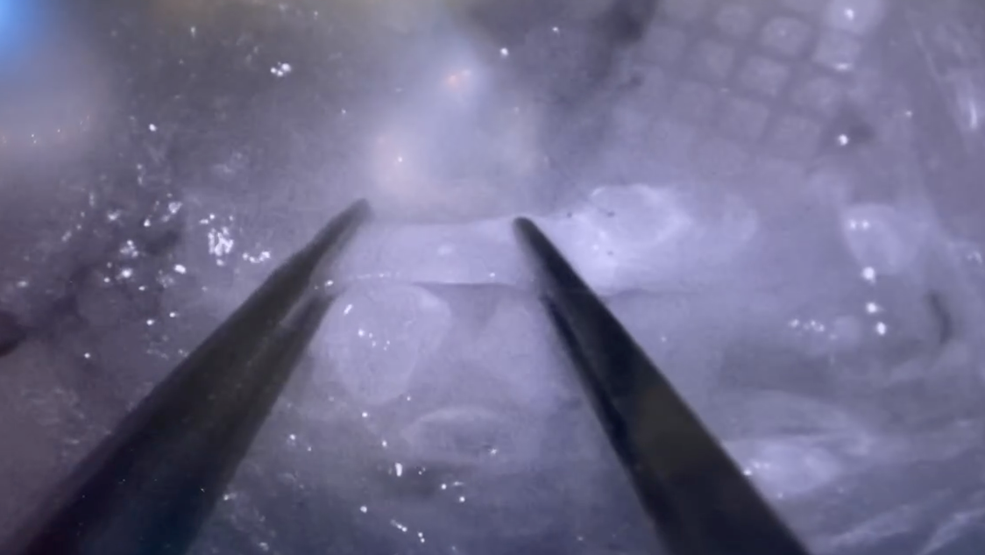
Figure 4D
Figure 4. Operative techniques in LVB. (A) Transection of the target lymphatic area should demonstrate lymphatic function. This is facilitated by subcutaneously injecting Isosulfan blue (Lymphazurin; United States Surgical Corp., Norwalk, CT) or methylene blue (American Reagent, Shirley, NY) along the fluorescent lymphatic pathway. (B) Intravascular stenting (IVaS) can be performed with nylon sutures prior to LVB. (D) an implantation technique implants the lymphatic into the venous lumen, using a stitch to connect lymphatic adventitia to venous intima. (E) The success of the bypass can be determined by direct visualization of the unidirectional flow of fluorescence from lymphatic into the recipient vein (distal to proximal) under microscopy.
In 2022, Bianchi et al. further noted that E-E had superior flow characteristics compared to side-to-end (S-E) and side-to-side (S-S). These findings contrast numerous reports corroborating S-E as superior to E-E, particularly in more advanced lymphedema.111,112 However, Kwon et al.’s results favoring S-E incorporated significantly higher ratios of lymphatics: RV in the S-E group than in the E-E group, possibly confounding their results. Yamamoto et al. reported that S-E and S-S unions outperformed E-S, often resulting in venous-lymphatic reflux and thrombosis.113 The authors cited that bidirectional drainage is a favorable dynamic, which remains controversial.101,113,114
A myriad of publications describes combinations and variations of these configurations, including
The surgical treatment of lymphedema must be combined with lifestyle interventions and postoperative compression. The most common recommendation is to avoid compression in the immediate postoperative period and instead encourage consistently elevating the affected limb though not more than 90 degrees.152,153 The patient can continue compression, lymphatic massage, and lymphedema therapy between 2-4 weeks postoperatively, taking care to avoid massaging incisions, and by one month, they can return to usual activities.152 The outcomes are improved by combining surgery with decongestive therapy, but patients often discontinue CDT postoperatively.154,155 The referrals and planning for post-ILR lymphedema surveillance are usually initiated preoperatively. The regimen after surgery consists of two weeks of decongestive therapy and activity limitations followed by a gradual return to range-of-motion exercises.34,143,146,147 In the first 24 months, patients are screened every three months by specialized physical medicine and rehabilitation physicians for the development of lymphedema via Lymphedema Index (L-Dex; Impedimed, Carlsbad, CA) bioimpedance and arm circumference measurements.156 Beyond two years, patients can be transitioned to bi-annual monitoring. Individuals with abnormal exams should be counseled to wear prescribed compression sleeves (20-30 mm Hg) during daytime hours and be instructed to return after six weeks of wear for retesting.
The quality and quantity of lymphedema outcome measures limit the evaluation of LVB efficacy.157 The objective measures of treatment include limb circumference and volume, which are the most comparable measures of treatment efficacy for lymphedema. Though these metrics are often criticized for being antiquated and unacceptably dynamic, the pooled effects of LVB are considered significantly efficacious in reducing limb circumference or volume.27,158 Objectively, LVB is associated with a pooled decrease in cutaneous infections.33 Finally, ILR is demonstrated to effectively reduce the risk of lymphedema as measured by a decline in prevalence, incidence, and relative risk.5,32,34,35,38,150,159,160
The subjective patient-reported outcomes (PROMS) are considered to “improve” after LVB, but metrics are considered too heterogeneous to compare and of universally poor methodological quality.27,30,41 The Consensus-Based Standards for the Selection of Health Measurement Instruments (COSMIN) analysis suggests that the PROMS with the best methodological quality included the lymphedema life impact scale (LLIS), Lymphoedema Functioning, Disability and Health questionnaire ([Lymph-ICF]; lower-limb specific [Lymph-ICF-LL]), patient benefit index-lymphedema (PBI-L), and upper limb lymphedema 27 (ULL-27).161-166
Future Directions
Lymphatic Surgical Training
There is yet to be formalized training for supermicrosurgery, which may create additional barriers to entry. To participate in training, expert microsurgeons can engage in a “line production method” for LVB with novice microsurgeons using a microscope and loupes, respectively, as these are demonstrated to increase the quantity and quality of LVB beyond those produced by a traditional single expert, single microscope approach.151 Papaverine can also prevent lymphatic spasms and reduce lag between novices and experts. Training models are constantly being improved and are demonstrated to support standard microsurgical instruments in anastomosis vessels of up to 0.3mm in an average of approximately 6 minutes.118,167-170
Physiologic and Biomechanical Research
The lymphatic function and contractile strength may be influenced by manipulation of the luminal size due to fibrosis or surgical technique. Unlike blood vessels, lymphatic vessels propagate fluid synchronously, contracting reminiscent of the cardiac cycle.171 The current understanding of the lymphatic circulatory system is that it 1) is a low velocity, low-flow system, 2) is composed of individually actively pumping lymphangions bounded by valves, 3) exhibits nonlinear flow or hysteresis, 3) collecting lymphatics exhibit Starling forces with a cyclical contraction (systole), positive transluminal pressure, and ‘suction pressure’ necessary for passive diastolic filling, and 5) is influenced by downstream, upstream, and external pressures.172 These recently uncovered features indicate the increasing complexity of lymphatics, which may predispose an unpredictable response to surgical interventions. The modern physiologic and biomechanical evaluation of lymphedema surgery in ex-vivo and in-vivo experimentation models lags behind clinical research. Testing these surgical procedures on animal models for lymphedema could enhance the scientific logic behind various practices in LVB.173-180
The scientific exploration of LVB dates back to the 1960s, during which several imaging methods were developed which permitted further surgical innovation. Over the last twenty years, LVB research has blossomed, driven by novel investigations of surgical techniques.6 The current practices of LVB are evidenced to impact patients’ lives positively, but inconsistent practices challenge the development of evidence-based guidelines and integration in treatment algorithms. Intradisciplinary standardization and high-quality comparative research are needed to inform LVB perioperative decision-making and reach a consensus.30,99,181
Authors’ contributions
Made substantial contributions to the writing of the original draft, review and editing, visualization, and project administration, and gave final approval of the version to be published: Daisy L. Spoer, MS
Made substantial contributions to the writing via review and editing and gave final approval of the version to be published: Lauren E. Berger, BA
Made substantial contributions to the writing via review and editing and gave final approval of the version to be published: Parhom N. Towfighi, MD
Made substantial contributions to the writing via review and editing and gave final approval of the version to be published: Karen R. Li, BS
Made substantial contributions to the conception and design of the study, writing via review and editing, supervision, and gave final approval of the version to be published: Laura K. Tom, MD.
Availability of data and materials
The data supporting this study's findings are available from the corresponding author, [L.K.T.], upon reasonable request.
Financial support and sponsorship
None.
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. This study was conducted with approval granted by the Georgetown-Medstar Institutional Review Board (IRB ID: STUDY00004860, 03/02/2022). All participants provided written informed consent.
Consent for publication
Participants provided written informed consent.
© The Author(s) 2022.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!
"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.
Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.
Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.
Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.
Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.
