AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2692-9562/029
*Corresponding Author: Priya Jeyaraj, Classified Specialist (Oral & Maxillofacial Surgery), Commanding Officer, Military Dental Centre (Gough Lines), Secunderabad, India.
Citation: Jeyaraj P. (2021) Sino-Maxillary Mucormycosis of Iatrogenic etiology in an immunocompetent patient - Importance of early diagnosis and prompt management; J Clinical Otorhinolaryngology 3(2); DOI: 10.31579/2692-9562/029
Copyright: © 2021, Priya Jeyaraj. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 11 March 2021 | Accepted: 29 March 2021 | Published: 05 April 2021
Keywords: mucormycosis; zygomycosis; phycomycosis; surgical debridement; amphotericin b; platelet rich fibrin (PRF)
Sino-maxillary mucormycosis is an opportunistic, aggressive, invasive and fulminant fungal infection, which has the ability to rapidly cross anatomical barriers, causing extensive hard and soft tissue destruction, leading to significant cosmetic deformity, functional debility and morbidity. It usually affects susceptible, debilitated or immunocompromised individuals. A comprehensive Review Paper is presented, with a descriptive report on an unusual Case presentation, involving the dentoalveolar complex which thereafter invaded the maxillary antrum, in an otherwise healthy, adult patient with nil comorbidities. A probable intraoral portal of entry, and a likely iatrogenic etiopathogenesis resulting from inoculation of the fungus or its spores during dental extractions carried out in an unsterile setting, has been considered and elucidated. An emphasis has been placed on according a high index of suspicion in diagnosis of this fungal infection even in immunocompetent and healthy adults, presenting with a seemingly simple, deceptively indolent odontogenic infection. The importance of careful, albeit rapid differential diagnosis, and a prompt and aggressive medical-surgical treatment protocol instituted immediately following a confirmatory diagnosis, helps in limiting the spread and degree of destruction which can be caused by this potentially lethal fungal infection.
Invasive fungal infections, otherwise referred to as mycoses, are uncommon, however when they do occur, they can be quite destructive, functionally debilitating, aesthetically deforming and devastating to patients. Mucormycosis is a rare opportunistic infection [1], which represents the third most common angio-invasive fungal infection, following candidiasis and aspergillosis, and is considered one of the most important medical complications in diabetics and immunocompromised patients. Mucormycosis, also referred to as Phyomycosis or Zygomycosis, is caused by a saprophytic aerobic fungus, belonging to the Class Phycomycetes / Zygomycetes; Order Mucorales; Family Mucoraceae and Genera Rhizopus, Mucor and Absidia [1, 2]. These opportunistic pathogens are ubiquitous organisms, existing in the environment, soil, air, food, bread molds, decaying vegetations, compost piles, animal excreta, and play a pivotal role in the cycle of decomposition in the natural world. Although majority of these pathogenic fungi require oxygen, they are capable of growing in anaerobic and microaerophilic conditions as well [2]. This organism is frequently found to colonize the oral mucosa, nasal mucosa, paranasal sinuses and pharyngeal mucosa of asymptomatic patients [3, 4].
These fungi do not usually cause disease in healthy people with intact immune systems, however, patients with predisposing immunosuppressive conditions may develop this invasive fungal disease [5]. These conditions include diabetes mellitus, renal failure, liver cirrhosis, malignancies, intravenous drug abuse, malnutrition states, stem cell transplants, immunosuppression, systemic corticosteroid therapy, neutropenia and hematological malignancies like multiple myeloma, leukemia and lymphoma [6-8]. It is likely that the hyperglycaemia state in diabetics stimulates fungal growth, and the reduction in chemotaxis and phagocytic efficiency in immunosuppressed conditions permit these otherwise innocuous organisms to proliferate. In the past decade, cases of mucormycosis have even been described in immunocompetent/otherwise healthy individuals, with no identifiable risk factors [9, 10].
Mucormycosis generally presents as an acute infection manifesting in rhinocerebral, pulmonary, gastrointestinal, cutaneous, or disseminated forms [11]. These opportunistic infections occur when the causative fungal organisms, to which we are frequently exposed [10], gain entry into the body due to a decrease in host defenses or through an invasive portal. The infection usually begins in the upper nasal turbinate or paranasal sinuses due to inhalation of fungal spores, or less commonly in the palate or pharynx. It can spread to orbital and intracranial structures either by direct invasion or through the blood vessels. The fungus invades the arteries leading to thrombosis that subsequently causes necrosis of hard and soft tissues. Tissue necrosis, often a late sign, is a hallmark of mucormycosis, resulting from angio-invasion and vascular thrombosis [11].
Rhinocerebral mucormycosis [12] is capable of producing widespread involvement of the oral cavity, maxilla, palate, nose, paranasal sinuses, orbits and central nervous system. Early symptoms of this disease include facial cellulitis, periorbital edema and nasal inflammation, followed by widespread tissue necrosis. Failure of prompt medical and surgical intervention may lead to cerebral spread, cavernous sinus thrombosis, septicemia and multiple organ failure lending to high morbidity and mortality.
The case of Sino-maxillary oral mucormycosis reported in this paper, was out of the ordinary in its presentation on two accounts. Firstly, its development following a dental extraction, which was indicative of the dental extraction site as the likely but unusual portal of entry of the causative pathogen. Secondly, it’s surprising occurrence in an immunocompetent and healthy adult, which added to the diagnostic and therapeutic dilemma of the case.
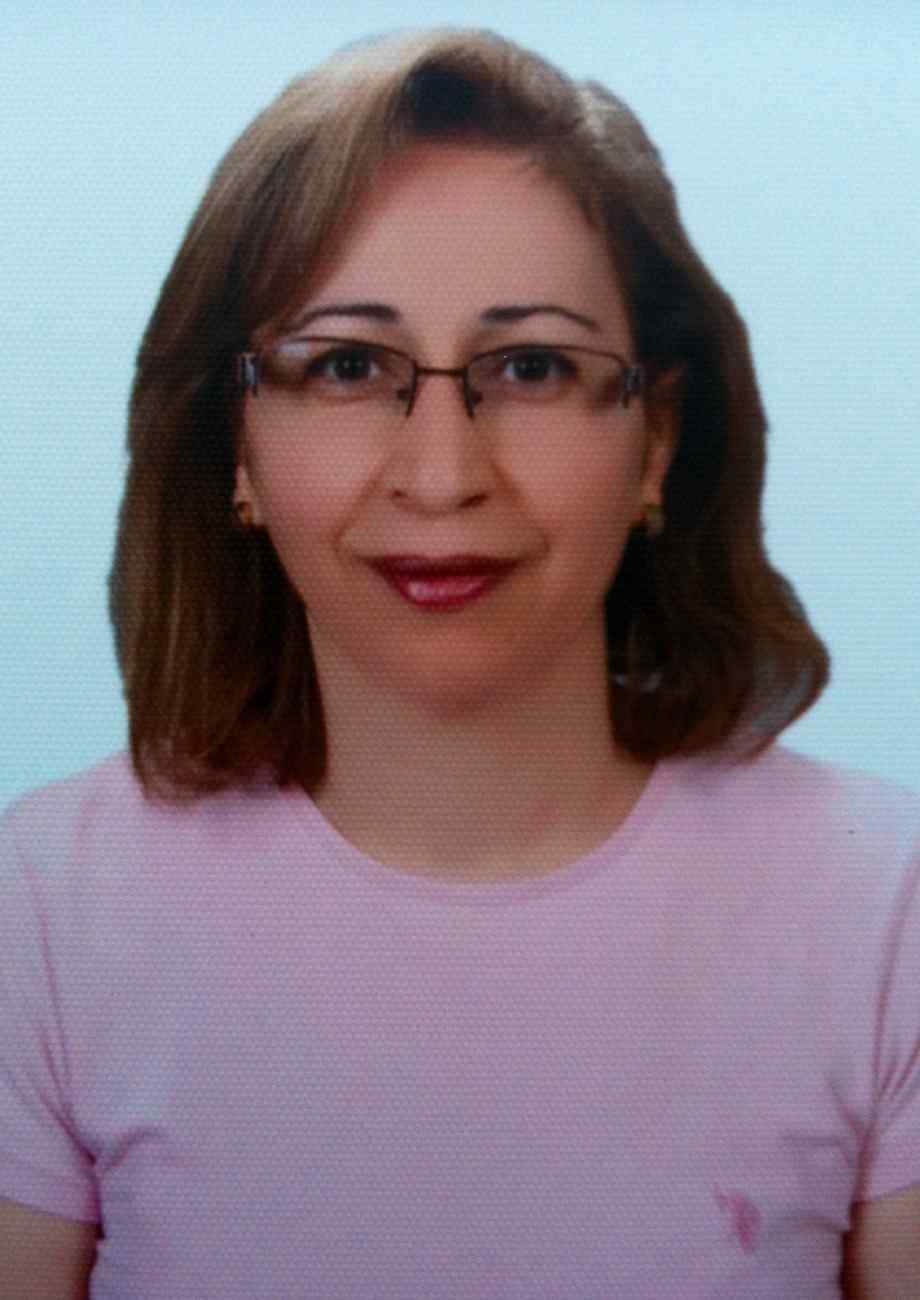
A 62-year-old male patient (Figure 1) reported with the complaint of non-healing extraction sockets of upper molar teeth on the right side, which had been extracted 3 months ago. He also complained of an occasional foul smelling discharge from the area and a troublesome nasal regurgitation of orally ingested fluids. In addition, he had also been experiencing a heaviness and dull ache in the region of the right maxillary sinus, which radiated to the right temple.
Figure 1: A 62-year-old healthy, immunocompetent patient who presented with a persistent post-extraction pain in the upper right quadrant, vague and dull pain and a feeling of heaviness in the region of the right maxillary sinus, accompanied by nasal regurgitation of orally ingested fluids via an oroantral communication, for the past three months. The complaints had developed following multiple upper dental extractions that had been carried out in an non-sterile setting at a rural clinic. (D, E) Radiographs (Para Nasal Sinuses view and Postero-Anterior view of skull) revealed a distinct haziness and opacification of the right maxillary antrum. (F) Intraoral examination revealed poor oral hygiene and a persisting oroantral fistula in the region of extraction socket of tooth 16. (G) Orthopantomogram revealed irregular bony destruction in the region of right maxillary quadrant and reduced periodontal support of the anterior teeth in the region. (H) A Gutta percha point placed in the incompletely healed extraction socket of 16, could be seen entering well within the right maxillary antrum, confirming the presence of an oroantral communication.
History revealed that he had been to a dental surgeon in a rural area three months ago for evaluation of several loose upper teeth. The mobility of multiple upper teeth was assumed to be due to their poor periodontal condition and lack of adequate tooth support resulting from chronic periodontitis. Hence, multiple dental extractions had been carried out in one sitting, without any flap reflection or osseous surgery. The patient’s post extraction course was protracted and painful which made him seek management by us.
On examination, the patient was afebrile with no visible swelling or features of acute inflammation (Figure 1 A-C). He was partially edentulous with multiple missing maxillary (17, 16, 15, 27) as well as mandibular (37 and 47) teeth. He had poor oral hygiene, with generalized periodontitis involving the remaining standing teeth. There was an oro-antral fistula in the edentulous right molar region (Figure 1F), presence of which was confirmed by inserting a Gutta percha point into the defect and taking radiographs thereafter (Figure 1G, H). Purulent material was seen draining intraorally though the fistula. Nasal regurgitation of water was also observed when he was asked to rinse his mouth, further confirming the oro-antral communication. The remaining teeth (18, 11, 12, 13 and 14) of the right upper quadrant were tender on percussion and exhibited Grade 3 mobility. The palatal mucosa appeared normal. Clinical presentation was suggestive of right maxillary sinusitis in relation to a residual oroantral fistula, which had developed following multiple dental extractions.
An Orthopantomogram (Figure 1G, H) showed irregular bony destruction presenting as a moth-eaten appearance, of the right maxillary alveolar region in relation to teeth 11, 12, 13 and 14, with clearly evident loss of their bony support. There was also noted a haziness and radiopacity of the right maxillary antrum, while the left side appeared normal. Paranasal Sinuses (PNS / Water’s) view and Postero-anterior (PA) view radiographs of the skull (Figure 1 D, E) too demonstrated a diffuse haziness and opacification of the entire right maxillary antrum. Differential diagnosis included acute Maxillary sinusitis, post-extraction bacterial / fungal maxillary infection and Osteomyelitis of the right maxilla.
The patient did not give any history of a possible immunosuppressed state such as Diabetes mellitus, organ transplantation, immunosuppressive therapy, malignant disease, chemotherapy, irradiation, etc. A complete work up was carried out to assess the immunological status of the patient and to check for the presence of any comorbidities, such as leukemia, malignancy, chronic obstructive pulmonary disease (COPD), etc., all of which were ruled out. A full workup of serum glucose, electrolytes, blood chemistries and blood gases was carried out and Diabetes mellitus was ruled out. Leukocytosis was noted with larger numbers of lymphocytes, suggestive of a chronic infection.
A scraping was taken from within the oro-antral fistula, including some tissue curetted from within the right maxillary sinus, for carrying out histopathological examination (Figure 2). Light microscopic evaluation of Haematoxylin and Eosin stained sections of the biopsy specimen revealed ulcerated pseudostratified sinus epithelium with underlying edematous chronically inflamed stroma (Figure 2 A, B) with numerous large colonies of broad, ribbon-like aseptate fungal hyphae branching at acute and right angles; and their spores (Figure 2 C-E). Vascular inhabitations by the hyphae were also noted within the large areas of necrosis. To further confirm the fungal infection, Fungal silver stain, namely the Grocott and Gomori methenamine silver (GMS) stain [14, 19] was employed for the remaining tissue specimen. The fungal cell wall appeared dark brown, almost black, while the surrounding tissue appeared green (Figure 2 F). This confirmed the diagnosis of Mucormycosis (Phycomycosis, Zygomycosis).
Figure 2: Figure 1. Histological analysis of tissue scrapings taken from the oroantral fistula and specimen fragments of the antral lining, confirming the diagnosis of Mucormycosis (Magnifications X50, X80, X100, X150). (A, B) (Haematoxylin & Eosin X 50) showing ulcerated ciliated, pseudostratified sinus epithelium with underlying edematous and inflamed stroma, chronic inflammatory cell infiltrate, thrombosed vascular channels, focal areas of haemorrhage and large areas of necrotic tissue with evident cellular degeneration and debris. (C, D, E) (Haematoxylin & Eosin X 80, X100, X150) Multitudes of large colonies of aseptate fungal hyphae branching at right angles (900), and their spores. The fungal colonies comprised of non-pigmented, wide (10 to 20µm), thin-walled, ribbon-like hyphae with few septations (pauciseptate) and right-angle branching. A few vascular channels were seen with inhabitation by the fungal hyphae and spores. (F) Grocott methenamine-silver staining (magnification X150) of biopsy tissue specimen showing dark brown fungal hyphae with a right–angle branching, in a greenish tissue background, confirming the fungal organism to be of the order Mucorales.
A CT Scan was performed for evaluation of the extent of involvement (Figure 3). 3-D reformatted images showed irregular destruction of the maxillary bone in the right upper quadrant, which included the alveolar region as well as the anterolateral wall of the right maxillary antrum (Figure 3A). On coronal and sagittal sections (Figure 3B, C), the antral lining on the right side showed radio-dense, polypoid thickenings, giving it a corrugated appearance; and the entire maxillary antrum appeared homogeneously opacified, while the contralateral maxillary antrum appeared uninvolved. The medial wall of the right antrum /lateral wall of the nasal cavity appeared to pushed medially, however there was no breach or bony destruction. The nasal cavities, ethmoid and frontal sinuses, orbital floor and the left maxillary antrum appeared normal and uninvolved (Figure D, E).
Figure 3: Non-contrast computed tomographic (NCCT) scans of the maxillofacial region. (A) 3-D reformatted images showing irregular bony destruction in the right posterior maxillary dentoalveolar region, extending to involve the lateral wall of the maxillary antrum, creating a wide oroantral communication via the necrosed and enlarged extraction socket of 16. (B) Coronal sections showing a distinct thickening and polypoid enlargements in the schneiderian membrane of the right maxillary sinus, giving it a corrugated, radio-dense appearance. The breach in the lateral sinus wall leading to the oroantral fistula is clearly evident. More posteriorly, the entire antrum appears to be diffusely and homogeneously opacified and obliterated by soft tissue mass. The ethmoid sinuses appear uninvolved. No bony disruption or breach detected in the orbital floor or lateral nasal wall, with nil evidence of orbital or nasal cavity extension. (C) Sagittal sections through the right and left maxillary antra showing a contrasting appearance of their interior, which appears diffusely opacified and obliterated on the right, whereas clear and uninvolved on the left side. (D) Axial sections showing obliteration of the right maxillary antrum by a homogenously enhancing soft tissue density, destruction of portions of its anterolateral wall, with uninvolved antral floor, palatal bone, and antral roof / orbital floor. The lateral wall of the right nasal cavity appears to be pushed medially, however no breach in the bone is detectable. The contralateral / left maxilla, orbits and ethmoid sinuses appear uninvolved.
Treatment planned for the patient aimed at an aggressive medico-surgical combination treatment protocol [13], comprising of antifungal chemotherapy coupled with thorough surgical local debridement of all necrotic tissue, to completely eradicate the fungal pathogen. Surgical intervention was planned under general anaesthesia, and included extraction of all remaining teeth of the right maxillary quadrant; removal of the necrotic soft tissue slough and sequestrectomy of loose, necrosed bone in the region; removal of the antral polypoid enlargements; surgical debridement of the entire right maxillary antrum with complete extirpation of the sinus lining, antral curettage and lavage; antral irrigation with an antifungal agent; placement of fresh autologous platelet rich fibrin within the surgical defect; and closure of the oroantral communication.
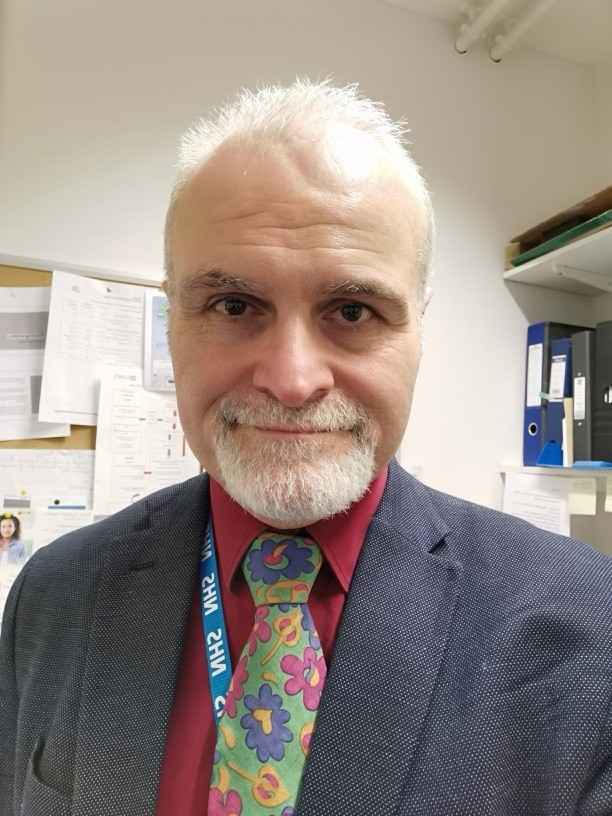
The patient was operated under general anaesthesia (Figure 4). A full thickness buccal mucoperiosteal flap was raised, exposing the entire right dentoalveolar complex and anterolateral wall of the maxillary antrum (Figure 4 A-C). The mucosal lining of the oroantral fistula was carefully excised. All loose bone fragments were removed from the region and necrosed margins of bone were nibbled using bone rongeurs. Extraction of the remaining standing teeth of the upper right quadrant was carried out (Figure 4 D, E).All necrotic material (Figure 4 F-H) was curetted out and sequestered bone pieces were carefully removed, which led to exposure of the interior of the right maxillary antrum. The antral lining was found to be thick and fibrous, with multiple polypoid growths, all of which were carefully curetted out (Figure 4 I-L). Maxillary sequestrectomy and debridement, extirpation of the entire antral lining, antral curettage and lavage were carried out (Figure M-O). A lipid preparation of Amphotericin B was used to irrigate the maxillary antrum to destroy any remaining fungal spores and to discourage any subsequent fungal proliferation. Fresh autologous platelet rich fibrin was prepared intraoperatively using a centrifuge, and was placed within the surgical site to encourage subsequent soft and hard tissue healing and regeneration (Figure 4P-R). The mucoperiosteal flap was then replaced and the wound closed. (Figure 4 S, T).
Figure 4: Intraoperative photographs. (A-C) Long crevicular incision extending from tooth 21 to 18 placed, with vertical buccal relieving incisions at either end. Full thickness mucoperiosteal flap raised exposing the dentoalveolar complex and anterolateral wall of the right maxilla. Irregular bone destruction and the wide oroantral communication seen in the 16, 17 region. (D, E) Mucous membrane lining oroantral fistula, excised followed by extraction of remaining teeth of the right upper quadrant. (F-H) Greyish white eschar and necrotic material seen in the posterior part of operative field, which was carefully curetted out. (I-L) Antral polyp-like soft tissue masses excised from within the right maxillary antrum. (M, N) Sinus lining extirpated, followed by thorough antral curettage and lavage to ensure elimination of all tissue and necrotic debris likely to contain fungal colonies and spores. (O) Necrotic margins of bone nibbled from the walls of the antrum, thus completing the sequestrectomy and debridement. A final irrigation of the antrum was carried out with a lipid solution of Amphotericin-B. (P-R) 20 ml of fresh autologous Platelet Rich Fibrin (PRF) prepared intraoperatively, using a centrifuge. PRF carefully placed within the surgical site, to encourage wound healing, and hasten subsequent bone and soft tissue regeneration. (S, T) Flap replaced and watertight wound closure carried out using interrupted Vicryl 3-0 sutures.
Postoperative recovery was smooth and uneventful. The patient was administered a single daily dose of liposomal Amphotericin B (1 mg/kg body weight/day) as an intravenous infusion in 100 ml of 5
Mucormycosis is the third invasive mycosis [2, 3] in order of importance after candidiasis and aspergillosis and is caused by fungi of the class Zygomycetes. Based on clinical presentation and the involvement of a particular anatomic site [12], mucormycosis can be divided into at least six clinical categories: (i) rhinocerebral, (ii) pulmonary, (iii) cutaneous, (iv) gastrointestinal, (v) disseminated, and (vi) miscellaneous. Chakrabarti et al. observed that rhino-orbito-cerebral type (44.2%) was the commonest presentation followed by cutaneous (15.5%) and renal (14.0%) involvement in their retrospective analysis for ten years in India [12]. The overall survival rate of patients with mucormycosis ranges from 50% to 85% with a higher survival rate of rhino-cerebral mucormycosis than pulmonary or disseminated forms as the rhinocerebral disease can frequently be diagnosed earlier, and the most common underlying cause, diabetic ketoacidosis, can be readily treated [13]. Notably, if the disease has not penetrated beyond the sinus, the prognosis is much better; indeed, in local sinonasal disease, the mortality has been reported to be less than 10% [14].
Early detection at the primary site, confirmatory diagnosis based on histopathology and culture, followed by a prompt and aggressive surgical
and antifungal treatment are imperative for successful management of this fulminant fungal infection.
The rhinomaxillary form of the disease, is a subdivision of the rhinocerebral form, and is usually caused due to inhalation of the fungus by a susceptible individual [15]. Inhaled spores cause disease in the upper and lower respiratory tracts of immunosuppressed persons. In immunocompetent or immunosuppressed hosts, spores can be inoculated into the skin and subcutaneous tissues by trauma, needle exposure, or insect bites, and they can be ingested, causing gastrointestinal disease 15, 16]. In rare instances, a dental extraction site may serve as an intraoral portal of entry by the fungus. The case of maxillary mucormycosis described in this report, affecting a healthy and immunocompetent individual, was most likely caused by inoculation of the virulent fungus or its spores at the time of dental extraction, which had probably been carried out in an unhygienic and unsterile setting. Another reason for high propensity of association of mucormycosis with extraction of maxillary posterior teeth can possibly be due to their proximity to the maxillary sinus [11], which often get involved when fungal spores are inhaled through nasal route.
Progression of the maxillary infection to the adjacent anatomical structures such as the nasal cavity, orbit, ethmoid sinuses, cranial cavity etc. can occur easily and rapidly, given the invasive and aggressive nature of this pathogen [14, 15, 16]. Fungal infection of the maxillary sinus can lead on to invasion of the nasal cavity through its lateral wall. Invasion through the maxillary antral roof / orbital floor can lead to orbital involvement, periorbital cellulitis, followed by the onset of conjunctival suffusion, blurry vision and even loss of eyesight. Orbital roof involvement can even serve as a portal of entry to the brain, with the fungus eroding through the floor of the anterior cranial fossa. Spread along the fascial planes and through the fascial spaces can produce facial numbness, soft tissue swelling, facial cellulitis, followed by eschar formation and ensuing necrosis of nasofacial region, unless prompt and effective management is undertaken [14]. Advancing infection can also spread from the ethmoid sinus to the orbit, resulting in loss of extraocular muscle function and proptosis with marked chemosis and can quickly result in cavernous sinus thrombosis, carotid artery, or jugular vein thrombosis (Lemierre syndrome) and death [16]. Hence, it is imperative to diagnose this condition quickly and effect prompt and definitive management to avert the possibly disastrous sequelae and complications of this extremely aggressive and invasive infection [17].
In routine maxillofacial practice, intra-oral exposed bone (maxillary necrosis) is generally diagnosed as osteomyelitis. Maxillary necrosis can occur due to bacterial osteomyelitis, herpes zoster, trauma, iatrogenic infections, or fungal infections, such as mucormycosis, aspergillosis, etc. A clinical suspicion of Mucormycosis requires confirmation by radiological and histological examination of a biopsy specimen [18]. Radiographs and CT scans of the maxillofacial region, showing irregular bony destruction accompanied by hyperdensity in the affected paranasal sinuses, schneiderian membrane thickening with or without polypoid growths, are highly suggestive fungal disease [19]. All these findings were observed in the case presented here (Figure 1; 3) and included unilateral maxillary sinus inflammatory changes and polypoid mucosal thickening of the antral lining. Radiologically, radio-opaque concretions may be identified in aspergillosis, whereas mucormycosis shows generalized opacification and a diffuse haziness of the sinus as was the case presented [16, 17].
Histopathological confirmation of the biopsy was confirmatory of the diagnosis of mucormycosis in the case presented. Tissue samples from the oroantral fistula and fragments of the lining mucosa of the affected maxillary antrum were screened, by subjecting them first to Haematoxylin and Eosin staining, followed by Grocott and Gomori methenamine silver staining. This dual screening of the tissue sample allowed the fungus as well as the host reaction to be clearly observed, enabling an accurate and rapid confirmatory diagnosis. This facilitated the infection to be managed immediately and effectively, before it involved the adjacent anatomical structures. Characteristic wide, ribbon like, aseptate hyphal elements that branched at right angles, were demonstrable in the scrapings taken from the oroantral fistula as well as in the sections of mucosal lining curetted from the right maxillary antrum. The fungal organisms were observed to be surrounded by extensive necrotic debris. Following surgical management, histological examination of the excised specimen of the extirpated schneiderian membrane as well as the necrotic tissue from the right maxilla, further confirmed the diagnosis.
Four factors or strategies are currently considered critical for eradicating Mucormycosis: rapidity of diagnosis; reversal, removal or reduction of the predisposing/risk factors (drugs or underlying diseases), appropriate surgical debridement of infected tissue, and rapid and aggressive antifungal therapy [14, 20]. Presence of necrotic bone acts as a nidus of infection, serving as a protective barrier for the organisms, thus preventing the effective action of systemically, administered antifungal drugs [14]. Thrombosis of blood vessels in the region may also reduce antibiotic effectiveness. So, surgical resection of involved hard and soft tissues and thorough debridement of all necrotic material has a very important role to play in effective management of this condition. Empirical parenteral antibiotic therapy with a broad spectrum [17, 18], covering Gram-negative and anaerobic bacteria, such as Cephalosporin and Metronidazole combinations are advocated in addition to antifungal medication, the drug of choice being Amphotericin-B, preferably the lipid formulation because adequate dosage can be delivered with reduced renal toxicity. Debridement of necrotic tissue in combination with medical therapy with antifungal drugs forms the basis of treatment. In consonance with the above management protocol, an aggressive medico-surgical approach was employed in our case as well, with excellent results.
Clinicians have reported the use of up to 7.5-10 mg/kg/d to treat mucormycosis, especially in CNS disease [18, 19]; however, the benefit of higher doses is unknown and such doses have a higher risk for nephrotoxicity. Amphotericin B deoxycholate can also be used for the treatment of mucormycosis, especially in settings of cost restraints. In our case, we employed a lipid preparation of amphotericin B administered at a dose of at 1 mg/kg/d, with good results.
Oroantral fistulas in such cases have usually been reported to have been closed by employing a double layered closure using a pedicled buccal fat pad and buccal advancement flap. buccal pad of fat advancement for closure of the oroantral fistula [21]. In our case, we employed a novel approach by placing fresh autologous PRF in the region of the bone defect at 16 and 17 region, before replacing and suturing the raised buccal mucoperiosteal flap. PRF helped to encourage bone and soft tissue regeneration in the dentoalveolar region, successfully sealing off the oroantral communication.
Prognosis of Mucormycosis of the Maxilla and Paranasal sinuses involves a high morbidity and mortality, owing to the rapid spread and extensive necrosis and destruction of contiguous vital structures by this invasive opportunistic pathogen. The severe functional debility and extensive cosmetic deformity it is capable of, makes it a formidable entity to manage effectively. The prognosis of a case definitely improves with a rapid and accurate diagnosis, prompt and early management by an aggressive and coordinated medical cum surgical protocol. High dose antifungal medication in combination with thorough surgical debridement, along with a concomitant reversal of the patient’s underlying risk factors and compromising medical conditions and / or immunosuppressive state, if any, comprise the mainstay of management.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!
"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.
Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.
Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.
Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.
Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti