AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2639-4162/124
North Manchester General Hospital, Department of Urology, Delaunays Road, Manchester, United Kingdom.
*Corresponding Author: Anthony Kodzo-Grey Venyo, North Manchester General Hospital, Department of Urology, Delaunays Road, Manchester, United Kingdom.
Citation: Grey Venyo AK, (2024), Prediction of Binding Affinity for some Tetrahydro carbazole Derivatives as Serotonin Receptor Antagonists from their Molecular Structural Descriptors, J. General Medicine and Clinical Practice, 7(3); DOI:10.31579/2639-4162/124
Copyright: © 2024, Anthony Kodzo-Grey Venyo. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 11 November 2023 | Accepted: 16 December 2023 | Published: 13 March 2024
Keywords: intraepithelial neoplasia; pein; penis; foreskin; glans penis; superficial; invasive; cancer; topical treatment; glans resurfacing; glansectomy; imiquimod; topical; laser
Penile intraepithelial neoplasia (PeIN) is a histopathology terminology that is utilized for precancerous penile lesions. PeIN is important in view of the high morbidity and mortality associated with progression to penile squamous cell carcinoma (PSSC). But PeIN is not commonly encountered and it does contribute to a limited evidence-base for the relative efficacy of available options of treatment. PeIN tends to be classified into HPV-associated and HPV-independent (differentiated) (dPeIN). Even though HPV-associated PeIN had been linked to the oncogenic effect of human papillomavirus (HPV), the HPV-independent pathway is stated to be driven by chronic inflammatory conditions. These two biology pathways had been iterated to be are associated with distinct histopathology examination features. The commonest morphology patterns of HPV-associated PeIN include basaloid, warty, and mixed PeIN. DPeIN is the morphological expression of HPV-independent PeIN. A review of therapy options and outcomes for PeIN, had summated the ensuing findings: Topical agents had demonstrated response and recurrence rates of 40% to 100% and 20% for imiquimod, and 48-74% and 11% for 5-fluorouracil, respectively. Discontinuation of topical agents in view of side effects had been noted in 12% of cases. Response rates for laser treatment options were 52 % 100%, with recurrence in 7 % 48% of cases and a change in penile sensitivity in 50%. Circumcision was documented to have cleared preputial PeIN. Recurrence rates pursuant to surgical treatment of glans PeIN were documented to be 25% for wide local excision, 4% for Mohs surgery, 5% for total glans resurfacing, and 10% for glansectomy. Limited data does exist related to the factors that would predict treatment response and to sequencing of treatment options. Many treatment options are available for men who have precancerous lesions of the foreskin or glans penis. Close follow-up is necessary inn view of the fact that PeIN lesions could or progress to invasive penile cancer, a close regular, follow-up assessments are required to establish early any recurrent PeIN lesion or the lesions that had become invasive or malignant. Considering the rarity of PeIN, and the fact that there is no global consensus opinion of the best treatment options of PeINs in various parts of the world it is important for all clinicians to be aware of the clinical manifestations, diagnosis, treatment options that may be available in every locality of the world including the developing countries taking into consideration the availability and non-availability of laser and other treatment agents. It is therefore important for readers to read carefully, summations related to PeINs of the penis in order to establish a quick diagnosis of the PeIN lesion so as to provide a suitable treatment for patients taking into consideration the local availability of treatment options.
Intraepithelial neoplasm an in situ epithelial squamous cell carcinoma of the skin that generally does not infiltrate the dermis or surrounding tissues has been iterated to have been first reported by Bowen. [1] [2] It had also been iterated that intraepithelial neoplasm most commonly manifests within the proximal skin of the trunk or limbs and it could also be found within the oral mucosa, conjunctival membrane, and nail bed [1] [3]. It has furthermore been stated that the aetiology may be related to chemical factors including arsenic agents and human papillomavirus [1] [4] Considering that intra-epithelial carcinoma of the penis is rare, it would be envisaged that a number of clinicians may not be familiar with the manifestations, diagnostic features, management, as well as outcome of the lesion. The ensuing article on intraepithelial carcinoma of the penis is divided into two parts: (A) Overview and (B) Miscellaneous Narrations and Discussions from some Case Reports, Case Series and Studies Related to Intraepithelial carcinoma of penis.
Aims
To review and update the literature on Penile Intraepithelial neoplasia (PeIN)
Internet data bases were searched including: Google; Google Scholar; Yahoo; and PUBMED. The search words that were used included: Penile Intraepithelial neoplasia; PeIN; Intra-epithelial neoplasm of penis; Intraepithelial neoplasm of glans penis; Intraepithelial tumour of foreskin; Intraepithelial tumour of penis. Fifty (50) references were identified which were used to write the article which has been divided into two parts: (A) Overview which has discussed various general aspects of Penile Intraepithelial neoplasms (PeINs) and (B) Miscellaneous Narrations and Discussions from some Case Reports, Case Series and Studies Related to Intraepithelial carcinoma of penis.
[A] Overview
Definition / general statements [5]
Essential features [5]
Terminology [5]
Epidemiology [5]
Sites
Aetiology
Clinical Manifesting Features
Diagnosis [5]
Diagnosis of intraepithelial neoplasia could be established based upon the ensuing: [5]
Prognostic factors
The prognostic factors of pen had been summated to include the ensuing: [5]
The development of frequent recurrence which has been iterated to constitute 48% of cases [20]
pen has been stated to be associated with low rate of progression to invasive carcinoma of 2%. [5] [20]
Treatment
The treatment of pen has been summated to include the ensuing: [5]
Gross description
The macroscopy examination features of pen had been summated to include the ensuing: [5]
Microscopic (histologic) description
The microscopy examination features of pen had been summated to include the ensuing: [5]
Immunohistochemistry staining features of pen (positive and negative)
Positive stains [5]
The positive immunohistochemistry of pen had been summated as follows: [5]
Negative stains [5]
The negative immunohistochemistry of pen had been summated as follows: [5]
Molecular / cytogenetics description [5]
The molecular / cytogenetics features of pen had been summated as follows: [5]
Differential diagnosis [5]
The differential diagnoses of pen had been summated as follows: [5]
[b] miscellaneous narrations and discussions from some case reports, case studies related to intraepithelial neoplasms of penis
Huang et al. [1] reported a 44-year-old Asian male patient who had gradually developed a ventral mass upon his penis 7 years preceding his manifestation. At first, the lesion measured about 1 cm in diameter and was occasionally accompanied by paraesthesia’s and bleeding after friction. He had normal micturition and he did not attend the hospital at first. When he developed an ulcer, he applied erythromycin ointment. Sometimes, his focal penile ulceration healed, but the condition often recurred. The scope of the lesion gradually increased over the preceding period of 7 years. Finally, he presented to the dermatology department of the hospital of the authors, where he underwent penile lesion tissue biopsy. The pathology report of the biopsy specimen revealed that he had penile intraepithelial neoplasia. Taking into consideration the large range of lesions, he came to the urological ward for admission and surgical treatment. The patient did not have any clear history of exposure to chemical properties such as arsenic. The result of his HIV antibody test was negative. He did not have a history of smoking or drinking of alcohol. The lesion was found on the ventral side of his penis and the total area of the lesion was about 2 cm ×2.0 cm (see figure 1A). The surface of the penile lesion was pale red with a grey edge. The penile lesion had an irregular shape and clear boundaries, and the lesion slightly protruded out of the surface of the skin. There was no obvious exudate from the ulceration, and there was no obvious redness or swelling of the encompassing skin.

Figure 1: Intraepithelial neoplasia lesion located on the ventral side of the penis (A). Complete resection of the lesion tissue on the surface of the penile deep fascia (B). The penile surgical area was covered with a pedicled scrotal flap (C). The shape of the penis after lesion resection and plastic surgery (D). The surgical area of the penis of the patient is not completely healed half a month after the operation (E). Penile morphology after complete wound healing (F). Reproduced from [1] Under the Creative Commons Attribution License, which allows reproduction of figures and contents of the Journal article provided the original source is cited and credited.
Pursuant to contiguous epidural anaesthesia, a skin incision line was marked at a 1.0 cm margin from the edge penile lesion of the patient. The scrotal flap range that was needed for the lesion to be isolated was set preceding the resection of the lesion. The skin of the lesion was cut vertically along the designed incision margin line, deep to the deep fascia layer, and completely resected the lesion upon the surface of the deep fascia (see figure 1B). Pursuant to achievement of careful haemostasis by bipolar coagulation, a 5.0 cm ×3.0 cm scrotal flap based upon the resected wound area was made and it was dissociated upon the surface of the deep fascia. With a formed pedicled scrotal flap, it was stretched to the ventral side of the penis and the surgical area of the penile skin was covered (see figure 1 C). Intermittent suturing of the subcutaneous tissue had reduced cavity formation and accumulation of local exudate (see figure 1D). The wound area was dressed in gauze under pressure, and the penis was wrapped up with a self-adhesive bandage under appropriate tension to promote wound healing. No drainage tube was inserted into the operational area. The bandage and gauze were removed to expose the wound and keep it dry 3 days pursuant to the operation. Pursuant to excision of the penile lesion excision, the wound was covered by scrotal flaps with blood supply. There was postoperative oedema within the penile wound without infection. During his follow-up assessment two weeks pursuant to the operation, the wound edge had not healed completely because of tension (see figure 1E). By means of care with wound dressing changes, the wound area finally healed (see figure 1 F). The pathology images (see figures 2 A and 2 B) demonstrated that the lesion tissue was covered with squamous epithelium and had demonstrated finger-like protrusion. The basal part of the lesion revealed bulbous advancing growth. The epithelium within the lesion area had severe dysplasia, disordered arrangement of polarity, large nucleus, deep staining, and complete basement membrane. No definite infiltration of basal layer tissue was identified. The lesion area revealed infiltration of polymorphonuclear giant cells and lymphocytes. The pathology diagnosis was penile intraepithelial neoplasia with granulomatous inflammation. No diseased tissue was identified at the margin of incision. During his 6 months of follow-up assessment, the patient did not have any recurrence of penile intraepithelial neoplasia and he did not have any obvious discomfort upon penile erection.
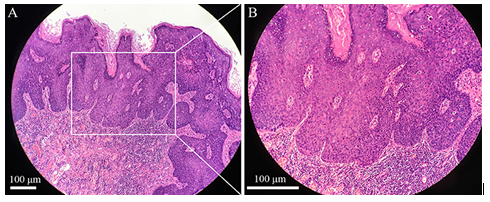
Figure 2: Pathological image of the penile intraepithelial neoplasia lesion with H&E staining, original amplification ×100, scale bar 100 μm (A). Pathological image of the penile intraepithelial neoplasia lesion with H&E staining, original amplification ×200, scale bar 100 μm (B). Reproduced from: [1] Under the Creative Commons Attribution License, which allows reproduction of figures and contents of the Journal article provided the original source is cited and credited.
Huang et al. [1] made the ensuing educative discussions:
Cañete-Portillo et al. [30] stated the following:
Cañete-Portillo et al. [30] undertook a study which was aimed to evaluate such a spatial relationship. Specimens were evaluated from circumcision that was undertaken in 28 cases, and penectomy that was undertaken in 81 cases. Cañete-Portillo et al. [30] reported that all cases had LLCs, penile intraepithelial neoplasia (pen), and/or invasive squamous cell carcinomas. Cañete-Portillo et al. [30] examined LLCs in relation to invasive carcinoma, pen, and normal epithelia. Invasive squamous cell carcinomas, classified according to the World Health Organization criteria as non-human papillomavirus (HPV)-related and HPV-related Cañete-Portillo et al. [30] reported their findings as follows:
Cañete-Portillo et al. [30] stated the ensuing:
Oertell et al. [13] stated that about 10% to 20% of all penile squamous cell carcinomas (SCCs) do originate within the foreskin, however, knowledge regarding preputial precursor and associated lesions is scant. Overtell et al. [13] undertook a study which was aimed to ascertain the prevalence of various precancerous and cancerous lesions exclusively affecting the foreskin, and to describe their pathological features. With regard the methods and results of their study, Overtell et al. [13] summated the ensuing:
Oertell et al. [13] concluded that the frequent coexistence of lichen sclerosus, squamous hyperplasia, differentiated PeIN and low-grade SCC had suggested a common non-human papillomavirus related pathogenic pathway for preputial lesions, and had highlighted the importance of circumcision in symptomatic patients for the prevention of penile cancer.
Chaux et al. [24] stated the following:
Chaux et al. [24] undertook a study which was aimed to test the usefulness of immunohistochemical p16 overexpression, which has been considered to be a surrogate for high-risk human papillomavirus infection, using this classification system. Chaux et al. [24] pathologically evaluated 141 patients with PeIN, associated (123 cases) and un-associated (18 cases) with invasive cancer. The distribution of PeIN types was found to be differentiated, in 72%; basaloid, in 9%; warty-basaloid, in 7%; warty, in 4%; and mixed, in 7%. Chaux et al. [24] also reported the following:
Chaux et al. [31] stated the ensuing:
Chaux et al. [31] undertook a study to seek an immunohistochemistry profile that could be helpful with regard to the classification and differential diagnosis of penile epithelial abnormalities and precancerous lesions utilizing the aforementioned system. The immunohistochemistry study panel included stains for p16, p53, and Ki-67. For p16 immunostaining study, only full-thickness positivity in all epithelial cells was considered as positive; for p53 and Ki-67 immunostaining, patchy or diffuse nuclear positivity above the basal layer was regarded as positive. Seventy-four lesions in 59 patients had been selected and classified as follows: differentiated PeIN, 34 cases; squamous hyperplasia (SH), 21 cases; basaloid PeIN, 15 cases; and warty PeIN, 4 cases. Chaux et al. [31] summarized the results as follows
Chaux et al. [11] reported the morphology features of 121 cases of atypical penile intraepithelial lesions. Chaux et al. [11] stated that the terminology penile intraepithelial neoplasia (PeIN) was utilized to encompass all of them, and the lesions had been classified into 2 major groups including: differentiated and undifferentiated groups. The latter was further divided into: warty, basaloid, and warty-basaloid subtypes. Ninety-five cases were found to be associated with invasive squamous cell carcinomas. Differentiated lesions had predominated accounting for 68% of cases, followed by warty-basaloid (14%), basaloid (11%), and warty (7%) subtypes. Multifocality was found in 15% of the cases. Differentiated lesions were found to be preferentially located within foreskin, whereas warty and/or basaloid subtypes were identified and noted to be more prevalent within the glans penis. The former lesions were preferentially observed in association with keratinizing variants of squamous carcinoma; however, the latter subtypes were found mostly in conjunction with invasive warty, basaloid, and warty-basaloid carcinomas. Lichen sclerosus was found to be present in 51% of cases of differentiated lesions and absent in warty and/or basaloid subtypes. Chaux et al. [11] summated that:
Canete-Portillo et al. [32] undertook a study to seek an immunohistochemistry staining profile that could be helpful in the classification and differential diagnosis of penile epithelial abnormalities and precancerous lesions utilizing the aforementioned system. The immunohistochemistry staining panel included stains for p16, p53, and Ki-67. For p16 immunostaining, only full-thickness positivity in all epithelial cells was considered as positive; for p53 and Ki-67 immunostaining, patchy or diffuse nuclear positivity above the basal layer was considered as positive. Canete-Portillo et al. [32] reported the following:
Velazquez et al. [33] stated the following:
Fernández-Nestosa et al. [18] stated the ensuing:
Fernández-Nestosa et al. [18] undertook a study which was aimed to detect and compare HPV genotypes in PeINs and associated lesions utilising high-precision laser capture microdissection-polymerase chain reaction and p16INK4a immunostaining. They evaluated resected penile specimens from 8 patients and they had identified 33 PeINs and 54 associated lesions. The commonest subtype was warty PeIN, followed by warty-basaloid and basaloid PeIN. Associated lesions that were found in the study were classical condylomas (17 cases), atypical classical condylomas (2 cases), flat condylomas (9 cases), atypical flat condylomas (6 cases), flat lesions with mild atypia (12 cases), and squamous hyperplasia (8 cases). Following a comparison, identical HPV genotypes were identified in pen and associated lesions in most of the patients (7 of 8 patients). HPV16 was the commonest genotype found present in both PeIN and corresponding associated lesion (50% of the patients). Non-specific flat lesions that contained mild atypia, classical condylomas, and atypical condylomas were the type of associated lesions that were most commonly related to HPV16. Other high-risk HPV genotypes that were found in PeIN and associated non-specific flat lesion with mild atypia were HPV35 and HPV39. They also stated that within their study of HPV in the microenvironment of penile precancerous lesions, they had identified identical high-risk HPV genotypes in pen and classical, flat, or atypical condylomas and, specially, in nonspecific flat lesions with mild atypia. They furthermore iterated that it is possible that some of these lesions represented hitherto unrecognized precancerous lesions
Fernández-Nestosa et al. [34] stated the following:
Fernández-Nestosa et al. [34] undertook a study which had a primary purpose of classifying PeIN morphologically, detecting HPV genotypes and determining their distribution according to PeIN subtypes. Their secondary aim was to evaluate the p16INK4a immunostaining as a possible HPV surrogate for high-risk HPV infection in penile precancerous lesions. The samples consisted of 84 PeIN cases, part of a retrospective cross-sectional analysis of 1095 penile carcinomas was designed to estimate the HPV DNA prevalence in penile cancers utilising PCR and p16INK4a immunostaining. Penile Intraepithelial Neoplasia (PeIN) was classified in HPV-related (basaloid, warty-basaloid, warty, hybrid, and mixed subtypes) and non-HPV-related (differentiated), the former was the most frequent. PeIN subtypes were differentiated (non-HPV-related) and basaloid, warty-basaloid, warty, hybrid and mixed (HPV-related). Basaloid PeIN was the most commonly diagnosed subtype, and HPV16 was documented as the most frequent HPV genotype they had detected. Warty-basaloid and warty PeIN had shown a more heterogeneous genotypic composition. Most HPV genotypes were found to be high-risk but low-risk HPV genotypes were also found present within a few cases (4%). A single HPV genotype was identified in 82% of HPV positive cases. On the contrary, multiple genotypes were found in the remaining 18% of cases. They iterated the following:
Canete-Portillo et al. [35] stated the following:
Hoekstra et al. [9] undertook a study to determine the incidence of penile intraepithelial neoplasia in the Netherlands utilising a nationwide histopathology registry and to discuss the nomenclature of premalignant penile lesions.
Hoekstra et al. [9] collected data from patients in the Netherlands who were diagnosed with a premalignant penile lesion between January 1998 and December 2007 from the nationwide histopathology registry (PALGA); this database covered all pathology reports of inhabitants in the Netherlands. The premalignant lesions included were erythroplasia of Queyrat; Bowen's disease; bowenoid papulosis; mild, moderate and severe dysplasia; and carcinoma in situ of the penis. The terminology that was utilised in the pathology reports was translated to penile intraepithelial neoplasia. The grading was made analogous to that of vulvar premalignant lesions. Hoekstra et al. [9] summarized the results as follows:
Aynaud et al. [36] evaluated the study of the existence of the morphology features specific for penile intraepithelial neoplasia (PIN), 1000 male sexual partners of women with genital condyloma or intraepithelial neoplasia. Aynaud et al. [36] presented ninety-two patients who had lesions that suggested intraepithelial neoplasia (pigmented or leukoplastic papules, keratinized condylomata, or erythroplastic macules) which underwent biopsy for histology and virologic studies. Aynaud et al. [36] summarized the results as follows:
Aynaud et al. [36] made the following conclusions:
Porter, et al. [37] stated the following:
Porter, et al. [37] undertook a study to describe the manifestation and treatment of patients who had PIN. Porter, et al. [37] described thirty‐five patients who had presented with PIN over a 7‐year period. Porter, et al. [37] summarized the results as follows:
Porter, et al. [37] made the following conclusions:
da Costa Nunes et al. [38] wrote an article to promote a literature revision of the relationship between the prevention of intraepithelial neoplasms (PeIN) and invasive penile cancer, and human papillomavirus (HPV) vaccination, aiming to enumerate the pros and cons of immunization. da Costa Nunes et al. [38] stated the following:
da Costa Nunes et al. [38] made the ensuing summations:
RMarkos et al. [39] made the ensuing summating discussions:
Deen et al. [41] stated the following:
Baldur-Felskov et al. [42] assessed the trends in incidence of penile cancer during 1978 and 2008 and high-grade penile intraepithelial neoplasia (PIN2/3) during 1998 and 2008 in Denmark. Baldur-Felskov et al. [42] estimated using two nationwide registries, age- and period-specific incidence rates. They used log-linear Poisson regression analysis to estimate average annual percentage change (AAPC) and 95% confidence intervals (CI). Baldur-Felskov summarized the results as follows:
Baldur-Felskov et al. [42] made the ensuing conclusions:
Gross and Pfister. [43] stated the following:
Wikström et al. [44] summarized the results as follows:
They concluded that PIN is highly HPV-positive, can show differing clinical pictures and is difficult to treat.
Fernández-Nestosa et al. [45] stated the following:
Cañete-Portillo et al. [30] stated the following:
Cañete-Portillo et al. [30] undertook a study to evaluate such a spatial relationship. They evaluated circumcision (28 cases) and penectomy (81 cases) specimens. All cases had LSc, penile intraepithelial neoplasia (PeIN), and/or invasive squamous cell carcinomas. Cañete-Portillo et al. [30] examined LSc in relation to invasive carcinoma, PeIN, and normal epithelia. Invasive squamous cell carcinomas, which were classified according to the World Health Organization criteria as non–human papillomavirus (HPV)-related and HPV-related PeIN, were present in 100 cases. Non-HPV-related (differentiated) PeIN was the commonest sub-type associated with LSc (89%). There were 5 spatial patterns which had been identified including: (1) LSc adjacent to PeIN (23%), (2) LSc adjacent and comprising PeIN (42%), (3) LSc next to and within invasive carcinomas (8%), (4) LSc throughout the sequence PeIN-invasive carcinoma (24%), and (5) LSc was separate (with normal tissue between the lesions) from PeIN and/or invasive carcinomas in a minority of cases (3%). Cañete-Portillo et al. [30] stated the following:
Guerrero et al. [46] stated the following:
Guerrero et al. [46] summarized their study as follows:
From 2000 to 2021, 55 surgical specimens of PSCC were identified. In all cases, thorough morphology assessment, HPV DNA detection, and p16, p53, and Ki-67 immunohistochemical (IHC) staining was undertaken. HPV-independent status was assigned based upon both negative results for p16 IHC and HPV DNA. Thirty-six of the 55 PSCC that amounted to 65% were HPV-independent. An intraepithelial precursor was identified in 26 cases out of 36 cases that amounted to 72%. Five of them that amounted to 19% had basaloid features, morphologically indistinguishable from HPV-associated HSIL. The median age of the 5 patients was 74 years and the ages of the patients had ranged between 67 years and 83 years. All 5 cases were p16 and DNA HPV-negative. Immunohistochemically, 3 cases had shown an abnormal p53 pattern, and had 2 shown wild-type p53 staining. The associated invasive carcinoma was noted to be basaloid in 4 cases and the usual (keratinizing) type in 1.
Guerrero et al. [46] made the ensuing conclusions:
Stojanović et al. [47] reported a case of a 36-year-old man who had a penile intraepithelial neoplasia who was evaluated at the Outpatient Clinic of the Department of Dermato-venereology Diseases of the Clinical Centre of Vojvodina in December of 2010. The patient was referred to the facility by a urologist and had histopathology reports of 4 biopsy-specimens taken from different plaques on his glans penis. Biopsy samples were collected from lesions which were clinically diagnosed as leukoplakia. The histopathology examination findings of all biopsy specimens had shown: “dysplasio epitheliiplanocellularis gradus levioris et partim gradus mediocris diffusa”. Given the histopathology diagnosis, the patient was referred to a dermatologist for conservative therapy of these lesions, avoiding radical surgery. During his admission, the patient had manifested with slightly indurated erythematous plaques with some desquamation at the surface, and a tendency for diffuse involvement of the entire glans penis. Topical 5% imiquimod cream was applied on the lesions once a day and was washed off after 8 hours during 10 weeks. Check-ups were scheduled for every other week in order to assess the course and progress of topical treatment. No significant side effects were observed, except for acute local inflammation which was accompanied by mild exudation and itching. After 10 weeks of treatment, complete regression of lesions resulted, and in the ensuing period of 18 months up to the time of publication of the article, no recurrence was observed
NUNES et al. [38] undertook a review which had the objective to promote a literature revision of the relationship between the prevention of intraepithelial neoplasms (PeIN) and invasive cancer of penis, and human papillomavirus (HPV) vaccination, which was aimed to enumerate the pros and cons of immunization. NUNES et al. [38] stated that their recent findings included the following:
Fernández-Nestosa et al. [18] iterated the ensuing:
Fernández-Nestosa et al. [18] undertook a study which was aimed to detect and compare HPV genotypes in PeINs and associated lesions utilising high-precision laser capture microdissection-polymerase chain reaction and p16INK4a immunostaining. Fernández-Nestosa et al. [18] evaluated resected penile specimens from 8 patients and they had identified 33 PeINs and 54 associated lesions. The commonest sub-type was warty PeIN, followed by warty-basaloid and basaloid PeIN. They classified associated lesions which included: classical condylomas (17 cases), atypical classical condylomas (2 cases), flat condylomas (9 cases), atypical flat condylomas (6 cases), flat lesions with mild atypia (12 cases), and squamous hyperplasia (8 cases). After a comparison, they found identical HPV genotypes in PeIN and associated lesions in the majority of the patients (7 of 8 patients). HPV16 was the commonest genotype present in both PeIN and corresponding associated lesion (50% of the patients). Non-specific flat lesions associated with mild atypia, classical condylomas, and atypical condylomas were the type of associated lesions that were most commonly related to HPV16. Other high-risk HPV genotypes that were present in PeIN and associated nonspecific flat lesion with mild atypia included HPV35 and HPV39. In their study of HPV in the microenvironment of penile precancerous lesions, Fernández-Nestosa et al. [18] identified identical high-risk HPV genotypes in PeIN and classical, flat, or atypical condylomas and, specially, in nonspecific flat lesions with mild atypia. Fernández-Nestosa et al. [18] iterated that it is possible that some of these lesions did represent hitherto unrecognized precancerous lesions.
Fernández-Nestosa, et al. [45] stated the ensuing:
Fernández-Nestosa, et al. [45] summarized the rest of their results as follows:
Fernández-Nestosa, et al. [45] made the ensuing concluding iterations:
Sabater-Marco et al. [48] described the association of balanitis xerotica obliterans and differentiated penile intraepithelial neoplasia (PeIN) with dermal elastosis and “bramble-bush” elastic fibres in a diabetic patient who had no history of penicillamine intake. Sabater-Marco et al. [48] reported an 84-year-old man who had presented with urethral obstruction syndrome which required postectomy, meatotomy, and foreskin excision. Histopathology examination of the specimen revealed changes of lichen sclerosus and differentiated PeIN. Orcein staining had shown striking dermal elastosis and trans-epidermal elimination of elastic fibres. At higher magnification, multiple serrations and buds arising from the borders of the elastic fibres were identified giving the so-called bramble-bush appearance. Sabater-Marco et al. [48] made the ensuing summating discussions:
Kristiansen et al. [50] analysed the incidence, treatment strategies and complications associated with penile intraepithelial neoplasia (PeIN) in Sweden over a period of 20 years. With regard to the materials and methods of their study, Kristiansen et al. [50] reported that data on PeIN from the Swedish National Penile Cancer Register were analysed regarding treatment in relation to age, size of the PeIN lesion, localization of the PeIN lesion and complications using chi-squared tests and logistic regression. They calculated the incidence of PeIN and age-standardized according to the European Standard population. Kristiansen et al. [50] summarized the results as follows:
Kristiansen et al. [50] made the ensuing conclusions:
Acknowledgements
Acknowledgements to Frontiers in Surgery for granting permission for reproduction of figures and contents of their journal article under the Creative Commons Attribution Licence; which allows reproduction of figures and contents of the Journal article provided the original source is cited and credited; which in this case is highly educative.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!
"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.
Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.
Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.
Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.
Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti
Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation. “The peer review process was efficient and constructive, and the editorial office provided excellent communication and support throughout. The journal ensures scientific rigor and high editorial standards, while also offering a smooth and timely publication process. We sincerely appreciate the work of the editorial team in facilitating the dissemination of innovative approaches such as the Bonori Method.” Best regards, Dr. Matteo Bonori.

I recommend without hesitation submitting relevant papers on medical decision making to the International Journal of Clinical Case Reports and Reviews. I am very grateful to the editorial staff. Maria Emerson was a pleasure to communicate with. The time from submission to publication was an extremely short 3 weeks. The editorial staff submitted the paper to three reviewers. Two of the reviewers commented positively on the value of publishing the paper. The editorial staff quickly recognized the third reviewer’s comments as an unjust attempt to reject the paper. I revised the paper as recommended by the first two reviewers.
