AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2690-4861/608
1 Neurology Department, Jamot Hospital Yaoundé, Cameroun.
2 Brain Research Africa Initiative, Yaoundé, Cameroon.
3 Endocrinology Department, Centre Médical la Cathédrale, Yaoundé, Cameroun.
4 Neurology Department, Central Hospital Yaoundé, Yaoundé, Cameroun.
5 Neuroscience Laboratory, Faculty of Medicine and Biomedical Sciences, The University of Yaoundé I, Yaoundé, Cameroon.
6 Internal Medicine Department, Jordan Medical Services, Yaoundé, Cameroun.
7 Internal Medicine Department, Aristide Ledantec Hospital, Dakar, Senegal.
8 Neurology Department, Yaoundé Military Hospital, Yaoundé, Cameroun.
9 Neurology Department, Centre Hospitalier Saint Nazaire, France.
10 Neuropediatric Department, Chantal Biya Foundation, Yaoundé, Cameroon.
11 Department of Pediatrics, Faculty of Medicine and Biomedical Sciences, The University of Yaoundé I, Yaoundé, Cameroon.
*Corresponding Author: Alfred K. Njamnshi, Brain Research Africa Initiative, Yaoundé, Cameroon.
Citation: Samuel E. Chokote, Gaelle Lemdjo, Leonard Ngarka, Gael Ananfack, Daniel Kollo, et al., (2024), Not Always an Infection: A Case Series of Immune-Mediated Encephalitis, Including the First Report of Hashimoto’s encephalopathy From Sub-Saharan Africa, International Journal of Clinical Case Reports and Reviews, 20(5); DOI:10.31579/2690-4861/608
Copyright: © 2024, Alfred K. Njamnshi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 12 November 2024 | Accepted: 10 December 2024 | Published: 31 December 2024
Keywords: autoimmune encephalitis; hashimoto’s encephalopathy; limbic encephalitis; neuromyelitis optica; sub-acute cognitive impairment
Encephalitis is a global health problem particularly frequent in Sub-Saharan Africa (SSA), where aetiologies are most often thought to be infectious despite the low microbiological yield. Some evidence suggests that autoimmune encephalitis (AE) could, however, be more prevalent than reported.
We report four (4) cases of immune-mediated systemic and non-systemic encephalitis, spanning across the large spectrum of this entity, presenting with a wide clinical and etiological heterogeneity. The first case is that of a 67-year-old lady with a three-month history of memory loss and abnormal behaviour. She was diagnosed with Hashimoto’s encephalopathy with a very good response on steroids. Case 2 is that of a 52-year-old man with an acute confusional syndrome with fever. He was diagnosed with encephalitis due to an undifferentiated connective tissue disorder responsive to immune therapy. The third case is that of a 14-year-old girl with a recurring history of motor deficits admitted for a rhomboencephalomyelitis due to neuromyelitis optica. Evolution was unfavourable in this case. The last case reports a 51-year-old male with an acute onset of behavioural abnormalities. MRI confirmed limbic encephalitis. Improvement was noted on steroids. The patient was lost to follow-up.
We discuss the context-specific challenges of identifying AE, mainly due to diagnostic technologies' financial and geographical inaccessibility (cerebral imaging, serological tests, antibody panels). The goal of this case series is to raise awareness among clinicians managing patients with encephalitis in SSA to look beyond infectious causes and consider AE especially in the presence of subacute cognitive impairment, inflammatory cerebrospinal fluid (CSF), and limbic involvement on brain imaging.
Encephalitis is a frequent diagnosis in Sub-Saharan Africa (SSA) in neurology, internal medicine, emergency and intensive care departments. A recently published review evaluating the global magnitude of encephalitis burden concluded that low-middle-income countries, including most countries of SSA, had the highest incidence worldwide (31.63/100,000 compared to 6.17 per 100,000 in high-income countries) [1]. Several studies have emphasized the challenges of etiological diagnosis of encephalitis in SSA [2,3]. In a multicentric series including patients from Rwanda, Uganda and Malawi presenting with an acute non-traumatic coma, a definite etiology was identified only in 37% of cases using conventional diagnostic techniques [4]. Historically, autoimmune diseases were considered to be rare in tropical Africa. This is evident in that a medline search with the keywords “Encephalitis” AND “Africa” yields data mainly on infectious causes. A scoping review of etiologies of encephalitis in 16 western African countries identified 21 pathogens. The authors argued that infectious causes are probably more common than non-infectious etiologies in tropical countries [5]. A more recent review series on Neuroimmunology in Africa equally underlined the scarcity of reported non-infectious causes of encephalitis [6,7]. However, a few studies suggest that auto-immune encephalitis could be as frequent as infectious cases and could etiologically account for a sub-group of “cryptogenic” encephalitis [8,9]. Data on inflammatory causes in sub-Saharan Africa are limited to a few case reports of autoimmune encephalitis from Kenya, Togo, South Africa and Soudan [10-13]. In these studies, only patients with antiNMDA and LGI1 were reported. As such, our setting might significantly underdiagnose the full spectrum of inflammatory encephalitis. This case series of four patients adds to recent data on immune-mediated encephalitis in sub-Saharan Africa, insisting on the diagnostic difficulties related to its wide clinical and etiological diversity and context-specific challenges to both diagnosis and management.
Case 1:
a 67-year-old right-handed lady and retired accountant, was referred by her attending endocrinologist to the outpatient neurology clinic for behavioural disorders. She was accompanied by her daughter, who reported a progressive onset of incoherent speech during conversations (without any logorrhoea) and psychomotor agitation with anterograde episodic memory loss over a period of two months before consultation. She had recently become verbally and physically aggressive, could not recognise familiar faces, and was disoriented in time and space to the point of becoming dependent on her children for most of her daily activities. Her daughter denied any hallucinations, insomnia, convulsions and fever. She had initially consulted a physician who diagnosed hyperthyroidism based on a very low ultrasensitive Thyroid Stimulating Hormone (TSHus) at 0.0012mUI/L (normal 0.4-4mUI/L and elevated total T4 and T3 hormones at 204.9 and 4.75 respectively (normal 4-12.5mcg/dl; 1.2-3.0nmol/l respectively. A contrast-enhanced cerebral CT scan revealed mild cortical atrophy but was otherwise normal. Despite the concern that the behavioural symptoms were not typical of hyperthyroidism, the endocrinologist initiated Carbimazole at 20mg twice daily (TID) and Propanolol at 40mg TID with rather worsening symptoms after a month. She was then referred to the psychiatric ward where Alzheimer’s dementia was diagnosed and started on Paroxetine and Mexazolam. Her persisting symptoms prompted the family to seek for a second opinion from our endocrinology clinic.
Her past medical history prior to the current illness was unremarkable. She denied consumption of alcohol or tobacco. There was no family history of psychiatric or neurologic diseases.
Her physical exam revealed an altered general state (WHO grade II) and normal vital signs (blood pressure: 123/69 mmHg, heart rate: 83 beats per minute, respiratory rate at 20 cycles per minute, temperature: 37.2°C). An evaluation of her higher mental functions revealed predominantly anterograde but also retrograde episodic memory loss, which was not improved by hinting. She equally presented apraxia, acalculia and was disoriented in time and space. Her mini-mental status examination score was 15/30. She had no cranial nerve palsies, no focal motor deficit, neither static nor kinetic cerebellar dysfunction. Her thyroid gland was not enlarged, and her physical exam was unremarkable. Hashimoto’s encephalopathy or paraneoplastic encephalitis was suspected, given the subacute cognitive impairment in the context of a biologically proven hyperthyroidism with persisting symptoms despite one month of treatment with antithyroid medications. Infectious, limbic encephalitis and Creutzfeldt Jacob disease were considered as differential diagnoses. A brain MRI was requested but could not be performed because of financial constraints. The CSF analysis was normal (proteins, 0.23g/l with no leucocytes, no germs on direct microscopy and sterile cultures). HIV, hepatitis B, C and syphilis serologies were all negative. Erythrocyte sedimentation rate was 28mm in the first hour (normal values lessthan 20mm), C-reactive protein was lessthan 6mg/l (normal values lessthan 6mg/l) and serum protein electrophoresis indicated a polyclonal hyperglobulinemia. Full blood count was equally normal. Antithyroperoxidase antibodies were very high at 600IU/ml (Normal value lessthan 34), as well as her TSH receptor antibodies at 6,60IU/ml (normal value lessthan 1.75). Antithyroglubulin antibodies were normal at 15IU1/ml). A thyroid ultrasound indicated bilateral nodules graded TIRADS 3. The left lobe showed two oval-shaped, moderately hyperechogenic nodules of mixed liquid and tissular content, 18 and 20mm in diameter, respectively. There were two similar nodules on the right lobe but of small size (12 and 5mm respectively). The total thyroid volume was normal at 11ml. Serum onconeuronal antibodies, and an EEG were equally requested but could not be performed due to financial limitations. Hashimoto’s encephalopathy was retained as the diagnosis and high dose steroids were started. She received 1g of Methylprednisone daily for five days intravenously with adjunct therapy. Her clinical state remained unchanged at the acute phase [6]. The induction therapy was followed by an oral relay at 1mg/kg/day of prednisone (60mg daily). Carbimazole was decreased to 40mg once daily [6]. After one month, her daughter on a phone call visit (the patient was out of town) reported improvement of her symptoms. She was less aggressive and more coherent and could recognize familiar faces. Two months post-hospitalization, she was brought in for an office control visit. Her general state and cognition were markedly improved. Her Mini Mental Status Examination (MMSE) score was normal at 27/30 (losing points only on immediate and delayed recall). The normalization of her overall condition (WHO grade 0) was highly in favour of Hashimoto’s encephalopathy following treatment with steroids. At this visit, her Free T4 (FT4) was mildly decreased at 7.4ng/l (N 8-19) with a slightly elevated TSHus at 6.438 mUI/L. Prednisone was slowly taken and stopped over the next three months without any worsening of her neurological condition. She is currently followed up at the endocrinology outpatient clinic with a normal thyroid function and no neurological abnormalities.
Case 2
a 52-year-old was admitted at the emergency department following a 24-hour history of abnormal behaviour, incoherent speech and psychomotor agitation with intense fatigue but no fever initially. At the emergency department he presented a tonic-clonic generalized seizure which lasted five minutes. His past medical history revealed he was a sickle cell disease trait carrier (Hb AS) with no acute crises. He had previously suffered gout crises but was not on treatment at the time of his admission. He was diagnosed with acute infectious encephalitis and started on Ceftriaxone 2 grams every 12 hours intravenously (IV), diazepam 10 mg stat IV and phenobarbital 200 mg every 24 hours intramuscularly (IM). A neurological consultation was requested to evaluate the persistence of his clinical condition three days after his admission. He had an altered general state (grade III of the World Health Organization classification) and a high-grade fever at 39.7°C with stage 2 hypertension at 169/100 mmHg. His neurological examination revealed a confusional syndrome with a Glasgow coma score of 14/15 (Eye opening: 4/4, verbal response: 4/5 and motor response: 6/6). There were no meningeal irritation signs. His pupils were normal and reactive to light, and there were no cranial nerve palsies or focal motor deficits. He equally had markedly symmetrically swollen and painful joints involving the proximal interphalangeal joints, the elbows, knees and ankles. Inflammatory encephalitis rather than infectious was suspected, especially considering the pattern of the concomitant joint involvement, which was atypical for a gout crisis. A brain CT scan and subsequent MRI scans were strictly normal. A post-ictal EEG showed non-specific diffuse delta slowing (see figure 1). CSF analysis showed mildly raised proteins at 0.62g/l (normal values 0.2-0.45g/l) and no cells. The C-reactive protein (CRP) was elevated at 48mg/l (normal lessthan 6mg/l), the erythrocyte sedimentation rate (ESR) was 29mm at the first hour (normal lessthan 20mm). The full blood count was normal. There was an acute kidney injury indicated by serum creatinine levels of 14.56mg/l (normal values 7-13mg/l), which subsequently normalized after 72 hours of IV rehydration. Serum electrolytes indicated a mild hypokalemia at 3.1mmol/l. There were signs of liver failure with a low prothrombin time at 56.7%, low serum albumin levels at 23.08g/l (normal values 34-54g/l), elevated liver enzymes (SGOT 63.50IU/l [lessthan 50UI/l] and SGPT 134.46IU/l [lessthan 50UI/l] and SGPT 134.46IU/l [lessthan 50UI/l]) and elevated total and direct bilirubin levels (145.35mg/l [normal value 12mg/l] and 84.38mg/l [normal value 2mg/l] respectively). Ferritin levels were equally raised at 1838.28ng/ml (18-270ng/ml). Normal blood and urine culture as well as a normal chest X-ray ruled out a sepsis. Though CSF Herpes simplex virus (HSV1 and 2) PCR could not be carried out, Herpes simplex encephalitis was ruled out with the normal brain MRI, the non-specific EEG pattern and the absence of cells in the CSF.
After consultation with an internist, inflammatory encephalitis due to an adult-onset Still’s disease was considered the most probable diagnosis as the patient fulfilled 2 major and 2 minor criteria of Yamaguchi diagnostic criteria [14]. A connective tissue disorder was considered as a differential diagnosis.
The patient was started on high-dose IV steroids (500mg of Methylprednisone daily for three days) with marked improvement in his overall clinical condition [6]. There was a complete regression of the confusional syndrome at day 9 of admission. Fever and joints inflammation signs equally regressed. The prothrombin time improved from 56 to 65%. The patient was discharged on day 12 with the provisional diagnosis of adult onset Still’s disease (while awaiting the results of the blood autoantibodies), on oral prednisone at 1mg/kg (80mg) with the usual adjunct therapy (calcium at 1000mg OD and vitamin D 800IU OD supplementation as well as a pantoprazole 40mg OD) At the one-month follow-up visit, the patient presented a deep venous thrombosis of the right popliteal vein for which rivaroxaban was administered initially at 15mg BID for 21 days, followed by 20mg daily. His antinuclear antibodies received at this visit were very high at 1/640 with negative anti ENA antibodies, native anti DNA antibodies as well as anticardiolipin, anti-beta 2 glycoproteins and antiprothrombin antibodies. A final diagnosis of an undifferentiated connective tissue disorder was deemed more probable than Still’s disease. The absence of symptoms and signs of dry eyes and mouth and oral and urogenital ulcers argued against Sjogren’s syndrome and Behcet’s disease respectively. Oral methotrexate at 7.5mg daily was added to his treatment. At the three-month follow-up visit, the patient was well, with no signs of a neurological or systemic relapse.

Figure 1: A 10 second EEG epoch showing diffuse generalised theta slowing at 5-6Hz with a one second burst of delta slowing at the 4th second (green arrow) indicative of a non-specific encephalopathy of mild to moderate severity.
Case 3:
a 14-year-old consulted at the neurology clinic for a rapidly progressive motor weakness of the left upper and lower limbs over a few days in an afebrile context. She had no headaches nor other signs of raised intracranial pressure. Her history indicated a similar weakness of the right hemi body for which she was admitted at another centre three months earlier. Her family history was unremarkable. A brain MRI performed at the time revealed supratentorial juxta cortical and periventricular white matter lesions and pontine, medullary and upper cervical lesions limited to C1 and C2 spine. None of these were contrast-enhancing. Her CSF was inflammatory with raised proteins (0.73g/l) and three leucocytes/mm3. No bacteria were identified on microscopic examination or after CSF cultures. Antinuclear antibodies, anti ENA antibodies were negative. She was treated with high dose steroids (1g of Methylprednisone for five days with a partial improvement of the right motor deficit which allowed her to be autonomous for most activities of her daily life. She was then discharged and was lost to follow-up.
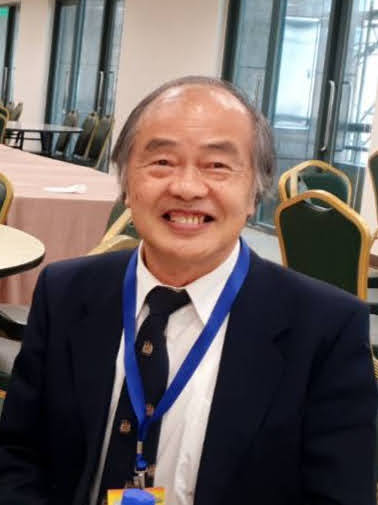
Physical examination at the author’s clinic revealed tachycardia at 100bpm, hyperpnea at 23cpm with a normal temperature and blood pressure at 37.3°C and 93/57mmHg. She was conscious, with a tetrapyramidal syndrome. On the right she had a proportional 4/5 motor deficit with brisk myotatic reflexes. On the left she equally presented a 3/5 proportional motor deficit. There were no sensory deficits. Cranial nerves exam revealed a left convergent strabismus and a right horizontal nystagmus The provisional diagnosis at this stage was a relapse of an inflammatory disease of the central nervous system. Another five-day course of high dose Methylprednisone (1g per day) [6] was initiated with potassium supplementation at 600mg BID, Omeprazol 20mg OD and Mebendazole 500mg stat. Her etiologic workup was completed with the search for oligoclonal bands in her CSF, anti-aquaporin 4 and antiMOG antibodies. Upon discharge (pending the aforementioned results), there was a significant functional improvement. Her muscle strength was 4/5 on the left upper and lower limbs, the right lower limb, and 5/5 on the right upper limb. At her one-week follow-up visit she presented her complementary CSF analysis which was negative for oligoclonal bands. Six weeks later, the patient presented with a one-week history of dysarthria and motor weakness of the left upper and lower limbs was well as the right upper limb. Another relapse was suspected. A control brain and spinal cord MRI revealed a 120mm long T2 and Stir hypersignal extending from the medulla oblongata to the C7 vertebra (see figure 2) with a marked increase of the antero-posterior cervical diameter (10-11mm). The brain MRI was normal. The patient was admitted for another high dose steroid course. Despite of first bolus (1g) of Methylprednisone her level of consciousness rapidly dropped to a GCS score of 6/15 (eye opening: 4, verbal and motor responses: 1). Her antiaquaporine 4 antibodies at this time were positive and anti-Myelin Oligodendrocyte Glycoprotein (MOG) negative. We concluded on a severe rhomboencephalomyelitis due to neuromyelitis optica (NMO). The absence of fever, and the relapsing nature of her symptoms argued against infectious causes such as tuberculosis and listeriosis. The patient was transferred to an intensive care unit for invasive respiratory support. High dose steroids were maintained at 1g/daily for a total of seven days and a first course of rituximab (1g) equally administered [15]. Her evolution was initially favourable with an improvement of her GCS to 15/15 on day 4 of admission. She subsequently developed a high-grade fever which was treated as a nosocomial infection. Despite being conscious, the patient could not be weaned off ventilatory support. She died on day 13 of admission at the ICU.

Figure 2: T2 sagittal brain and cervical spinal cord MRI showing a 5-segment-long (C1-C5) spinal hypersignal (red arrow) extending upwards to the medullary oblongata (green arrow)
Case 4:
A 51-year-old male was admitted at the emergency department for a rapid onset of diffuse intense headaches which began 24 hours prior to consultation. He was accompanied by his wife who reported having noticed on the same day, that her husband had some memory loss. The patient was logorrheic with incoherent speech and psychomotor agitation.
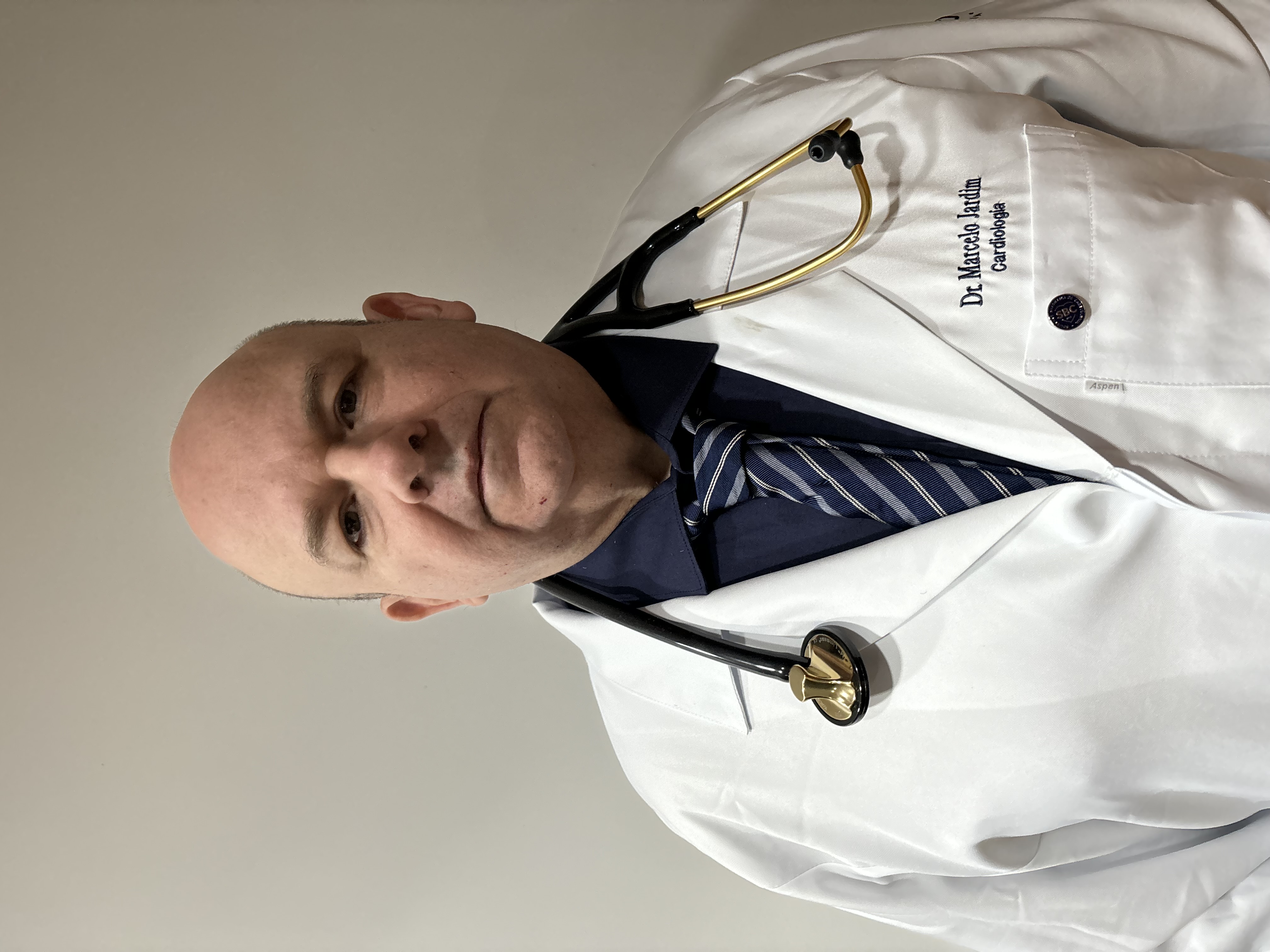
He had visual and tactile hallucinations as he insisted on seeing and feeling an electric discharge entering his body from the head. There was no nausea, vomiting nor fever. He had a three-month history of newly diagnosed type 2 diabetes already associated with length-dependent sensory polyneuropathy. He was non-compliant to Metformin which his endocrinologist had prescribed. His wife equally reported a history of chronic alcohol consumption. His physical examination revealed an altered general state (grade III WHO), a grade II hypertension at 166/97mmHg, a random blood sugar at 2.7g/l, a heart rate of 64 bpm and a temperature of 37°C. The patient was confused with a GCS of 14/15 (eye opening 4, verbal response 4, motor response 4). He had no meningeal signs, cranial nerve palsies or a motor or sensory deficit. Considering the recent onset of headaches, a subarachnoid haemorrhage or cerebral venous thrombosis were considered as differential diagnoses, coupled with an alcohol withdrawal syndrome. A contrast enhanced brain CT scan was normal but the brain MRI showed bilateral and symmetrical hippocampal T2 Flair hyperintensities with no gadolinium enhancement (figure 3). CSF was clear with a protein level of 0.49g/l, no cells nor bacteria identified. The patient’s full blood count, kidney function tests, liver enzymes, and serum electrolytes where within normal values. The CRP and D-dimer levels were mildly elevated at 12mg/l and 722ng/ml respectively. Limbic encephalitis was diagnosed considering the characteristic MRI pattern and the patient was started on high dose steroids (1g per day of Methyl prednisone) with adjunct therapy [6]. On the third day of treatment the patient was calm but still had incoherent speech. On day 5, the aforementioned hallucinations persisted and the steroid treatment was continued to day 7. The patient was discharged on oral prednisone at 1mg/kg (80mg) with calcium, vitamin D and pantoprazole. Antineuronal antibodies (antiLGI1, Caspr2, anti GAD, anti NMDA) and onconeuronal antibodies (anti Hu, Ri, Yo, Ma2 and antiamphyphysin antibodies) as well as thoraco-abdomino-pelvic scan were requested to investigate an autoimmune or paraneoplastic origin of the limbic encephalitis. The patient was however lost to follow-up.

Figure 3: 1.5 Tesla Brain MRI scans (case 4) A) Coronal and Axial B) T2 Flair sequences showing bilateral hypersignal in the medial temporal lobe structures.
This series presents multiple interests as it adds to the scanty literature on inflammatory encephalitis in SSA. Data on the subject is mainly limited to case reports and case series. Three cases of anti NMDA receptor encephalitis were reported from Kenya in 2019 by two teams [10,16]. A similar case each was described from Sudan and Togo in 2021 and 2022 respectively [11,13]. Izanne et al. also described a case of antiNMDA receptor encephalitis coupled with one case of LGI1 antibodies from South Africa [12]. Ndondo et al. reviewed several cases of Acute Disseminated Encephalomyelitis and COVID 19 acute necrotizing encephalopathy [17]. To our knowledge this is the first report from Cameroon and the central African sub-region. This increasing data should prompt health care professionals in SSA to consider non-infectious aetiologies of encephalitis in their clinical practice. There is mounting evidence that AE could be as frequent as infectious causes [7]. This is again plausible considering the low yield of microbiological CSF analysis of patients with meningitis or encephalitis even in developed countries with optimal resources [18]. Abboud et al. suggests diagnosing and treating autoimmune encephalitis after the exclusion of infectious aetiologies as well as metabolic and toxic causes, particularly in the setting of inflammatory CSF [8].
The originality of this paper is the presentation of almost the entire spectrum of inflammatory encephalitis, particularly in a context where the causes are empirically thought to be infectious. In its broad form, inflammatory encephalitis refers to all the conditions in which symptoms are related to immune-mediated inflammatory responses. Patel et al. proposed classifying systemic, non-systemic and post-infectious
immune-mediated encephalitis [19]. Systemic autoimmune encephalitis comprises connective tissue disorders, Hashimoto’s encephalopathy and neurosarcoidosis. Non-systemic conditions include idiopathic or paraneoplastic autoimmune encephalitis including neuromyelitis optic spectrum disorders (NMOSD) with target surface antigens against aquaporine 4 or antiMOG [8]. Our series therefore demonstrates the wide range of the full spectrum of immune-mediated both systemic and non-systemic encephalitis with which the clinician could be confronted. The neurologist should consider these different clinical scenarios when approaching patients with encephalitis.
Despite this clinical and etiological heterogeneity, the diagnosis of inflammatory encephalitis should follow a common algorithm as given by the diagnostic criteria for AE (Table 2) [20]. These include mostly acute or subacute evolution of symptoms frequently cognitive or neuropsychiatric (as with cases 1 and 3), supportive paraclinical examinations with brain imaging (MRI), EEG and CSF analysis. Other causes, particularly infectious should be ruled out with appropriate serological and polymerase chain reactions (PCR) exams and autoantibodies searched for in serum and CSF. This approach immediately underscores the challenges of diagnosing AE in many SSA countries. Firstly, the scarcity and high cost of MRI scans in the context where the cost of health care is endured mainly by the patient and his family. Ogbole et al. identified 84 MRI units for a combined population of 372,551,411 in West Africa (0.22 per million population) Most of these were low field strength systems [21]. Comparatively, Japan reported 51.67 MRI units per million population in the same study. Secondly, extensive serological and PCR tests for ruling out infectious causes are generally unavailable in several African countries. This is the same for autoantibody panels which are not only costly but often performed in specialised laboratories out of the country thus delaying the diagnosis as was particularly the case for the third patient of our series. In the Togolese study mentioned above, there was a three-week (23 days) delay between the request for CSF and serum NMDAr antibodies and the availability of the result [11]. Cases 1 and 4 in our series could not carry out all prescribed exams mostly because of financial limitations. In Cameroon for example, an AE antibody panel comprising anti Hu, Ri, Yo, Ma2, CV2, amphyphysin, NMDAR, AMPAR, mGluR1, mGluR5, glycine R, LGI1, Caspr2, DPPX and GABAB just in the serum costs altogether 2,000,000 FCFA (3210 US dollars). This largely surpasses the minimum wage of an average Cameroonian which was 36,270 FCFA (58.0USD) in 2024 [22]. As in similar situations, the neurologist and physician practicing in SSA must rely on a detailed clinical evaluation and a good clinical judgement to diagnose correctly [23]. In case 1 for example though HSV PCR examinations could not be done, Herpes simplex encephalitis was ruled out considering the normal brain MRI, non-specific EEG pattern and the presence of systemic signs (symmetric polyarthritis) which was the main clue for the diagnosis. Therefore, the SSA clinician should maintain a high level of clinical suspicion for AE particularly when faced with a subacute onset of psychiatric and behavioural disturbances [24], cognitive dysfunction [25], involuntary movements [26], intractable seizures [27], sleep disturbances [28], autonomic instability, and decreased level of consciousness [19]. Once infectious, metabolic and toxic causes have been ruled out, autoimmune encephalitis should be considered especially in the presence of CSF pleocytosis and despite the unavailability of serum and CSF autoantibodies. The 2016 AE clinical criteria emphasize the importance of early empirical immunotherapy once AE is highly suspected and infectious etiologies are excluded even in the absence of autoantibodies. The authors feel that this recommendation is especially relevant for good patient care in resource-limited settings such as ours [20]. That notwithstanding, improving the diagnoses of AE in SSA will require sensitisation not only of healthcare professionals but equally of policy makers, to improve economic access to care. In this regard, Cohen et al. had already underlined the high cost of diagnosing and managing patients with AE encephalitis with median hospital charges per admission ranging from 50 000 US dollars in non-ICU patients to 173 000USD in those admitted to the ICU [29].

Table 1: Summary of clinical and paraclinical findings

Table 2 Diagnostic criteria for possible autoimmune encephalitis (all three of the following criteria were met in our patients) [30]
The individual cases equally present specific interests. To the best of our knowledge, case 1 represents the first report of Hashimoto’s encephalopathy (HE) from sub-Saharan Africa. Although rare and somewhat controversial, HE should be considered as diagnosis in the presence of encephalopathy with no obvious aetiology or rapid onset cognitive decline even in the absence of clinical and biological signs of an abnormal thyroid function. In this series, neurological symptoms were attributed to Hashimoto’s encephalopathy rather than direct effect of hyperthyroidism mainly because of the persistence of symptoms despite one month of antithyroid medication and a favourable response on steroid medication in the context of high titres of antiTPO antibodies. Xu Huang et al. used a similar paradigm of diagnosing HE in a patient unresponsive after two weeks of antithyroid medication [31]. Misdiagnosis of HE for Alzheimer’s dementia as in case 1 of our series or for a viral encephalitis have equally been described in previous reports [32, 33]. Clinicians should keep this diagnosis in mind as it is highly treatable and steroid responsive. Neuromyelitis Optica is an inflammatory disease of the CNS that generally affects the optic nerve and the spinal cord. Brainstem involvement in NMO as was the case for the third patient in this series has recently been described in NMOSD and is seemingly more frequent in non-Caucasian populations [34]. The most frequent signs and symptoms were uncontrolled vomiting, intractable hiccups, cranial nerve palsies and pruritis. A recent systematic review in African series reported a prevalence of brainstem syndromes between 11-25% [35]. Overt encephalopathy with frank comatose state as was the case in our series is seemingly rare in literature. Case 4 emphasis the role of brain imaging in diagnosing inflammatory encephalitis. Though the clinical diagnosis was not specific, the MRI lesions were characteristic. According to the 2016 AE clinical criteria by Graus et al., the presence of bilateral limbic encephalitis is the only MRI finding sufficient to diagnose definite AE in the correct clinical setting (for example, negative CSF viral studies) even in absence of neuronal antibodies [20]. Unfortunately, the patient was lost to follow-up and a specific aetiology could not be identified.
The present case series has many limitations. Indeed, in most cases, all appropriate investigations according to international standards could not be carried out because of financial constraints or technical limitations. A brain MRI, EEG, thyroid scintigraphy would have improved diagnostic accuracy in case one. CSF viral PCR evaluations would have equally been necessary to rule out viral encephalitis in cases one to three formally.
This case series intends to raise awareness of clinicians on immune-mediated causes of encephalitis even in the tropical countries where most aetiologies are thought to be infectious. It underlines the clinical and etiological heterogeneity of this syndrome. Moreover, our report underscores the challenges, both financial and technical, faced by health professionals specifically practising in SSA in the diagnosis and management of inflammatory encephalitis. In most cases however, the prognosis could be favourable with immunomodulatory drugs thus the need to maintain a high index of suspicion in the face of acute/subacute cognitive or behavioural disorders for a timely and accurate diagnosis.
Consent for publication
The patients gave their consent agreeing to publication of the manuscript
The authors have no competing interests.
ESC, GL, GA, RN received the patient and did the initial management under the supervision of AKN. ESC and GA wrote the first draft of the manuscript. GL, LN, KD, FD, EM, NLN, YF, GT, HMA and AKN critically reviewed the first draft and validated the final manuscript. AKN took the decision to submit.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.
Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.
Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.
My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.
Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.
